What is already known
Immune checkpoint inhibitors (ICIs), which help the immune system recognize and fight cancer cells, have proved effective in treating melanoma, which is often resistant to traditional therapies. However, not all people with melanoma respond to these drugs, particularly those with advanced cancer. Previous research suggests that the gut microbiota influences responses to immunotherapy, but variability across studies indicates that focusing only on gut profiles may miss other important biological factors.
What this research adds
Over 13 months, researchers followed 23 people with advanced melanoma who were treated with ICIs, collecting both blood and fecal samples before each treatment. Specific microbial functions, such as those related to bacterial flagella and carbohydrate metabolism, were linked to improved treatment outcomes. Further analyses showed that certain gut microbes can stimulate immune responses by mimicking cancer-associated tumor antigens, enhancing the body’s immune reaction against the tumor.
Conclusions
The findings suggest that a beneficial gut microbiota may predict better responses to immunotherapy, potentially informing therapies or dietary interventions to improve cancer treatment.
Immune checkpoint inhibitors (ICIs), which help the immune system recognize and fight cancer cells, have proved effective in treating melanoma, which is often resistant to traditional therapies. However, not everyone respond to these drugs, particularly those with advanced cancer. Now, researchers have found that specific gut microbiota features correlate with better responses to immunotherapy in people with melanoma.
The findings, published in Cell Host & Microbe, suggest that a beneficial gut microbiota may predict better responses to immunotherapy, potentially informing therapies or dietary interventions to improve cancer treatment.
Previous research has linked a person’s gut microbes with their response to immunotherapy, but variability across studies indicates that focusing only on gut profiles may miss other important biological factors.
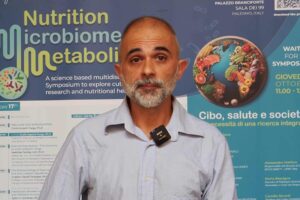
To better understand the connection between gut bacteria and response to ICIs, researchers led by Angeli Macandog at Istituto Europeo di Oncologia in Milan, Italy, followed 23 people with advanced melanoma over a period of 13 months, collecting both blood and fecal samples before each treatment. This approach allowed the team to track changes in the microbiota and immune markers linked to better treatment outcomes.
Microbial functions
About 55% of the study participants responded to ICI therapy, and in 74% of cases the cancer was stabilized.
The researchers identified bacterial species, such as Clostridia, that were linked to successful immunotherapy responses. They also found that specific microbial functions, including those related to bacterial flagella and carbohydrate metabolism, were associated with better outcomes.
These microbial functions were better at distinguishing responders from non-responders than individual bacterial species, which can vary based on diet, geography and other factors, the researchers say.
Mimicking antigens
People with melanoma who survived without disease progression for more than 24 months had more stable gut microbiotas over time. In contrast, people with shorter survival times showed more variation in their microbiotas.
Further analyses showed that certain bacterial proteins in the gut of responsive patients mimic tumor antigens. These proteins can trigger immune responses against the cancer by resembling known targets in melanoma cells. Laboratory tests confirmed that these bacterial peptides could bind to immune cells, activating them and boosting the body’s ability to target and destroy cancer cells.
The findings suggest that the gut microbiota can help train the immune system to recognize cancer more effectively, thus improving the outcome of immunotherapy.