What is already known
Gut bacteria can sway a person’s response to immunotherapy — a treatment that unleashes the body’s immune system to fight cancer. But the mechanisms by which the microbiota boost anticancer immune responses remain unclear.
What this research adds
Working in mice, researchers found that a specific population of immune cells allows beneficial gut bacteria to reach sites where anti-tumor T cells are primed to tumor-specific antigens. Once gut bacteria reached these sites, they amplified the immune stimulation generated by immunotherapy treatment and boosted T cells’ anti-cancer activity. Mice treated with antibiotics had fewer gut bacteria trafficking to tumors and a poorer response to immunotherapy.
Conclusions
The findings shed light on a general mechanism by which gut bacteria may influence anti-cancer immune responses.
Gut bacteria can sway a person’s response to immunotherapy — a treatment that triggers the body’s immune system to fight cancer. But the mechanisms by which the microbiota boost anticancer immune responses remain unclear. New work done in mice revealed that specific immune cells traffic gut bacteria to body sites where the microbes increase the anti-cancer activity of immunotherapy.
The findings, published in Science Immunology, shed light on a general mechanism by which gut bacteria may influence anti-cancer immune responses. “Our results could provide insight as to why different gut microbiota taxa or mechanisms are being espoused as critical for [immunotherapy] efficacy,” the researchers say.
A class of immunotherapy drugs called checkpoint inhibitors remove certain natural barriers to immune activity, unleashing a person’s immune system against tumor cells. But up to 50% of people do not respond to treatment. And although several gut bacteria, including Akkermansia muciniphila and Faecalibacterium prausnitzii, have been associated with increased responses to immunotherapy, it’s unknown how these bacteria can boost anti-cancer responses.
To investigate the microbiota’s role in cancer treatment, Andrew Koh at the University of Texas Southwestern Medical Center and his colleagues administered checkpoint inhibitor drugs to mice with or without melanoma tumors. Then, the researchers assessed whether gut bacteria moved into other body sites.
Shuttling microbes
After immunotherapy treatment, gut microbes traveled to lymph nodes in the abdomen, or mesenteric lymph nodes. Lymph nodes are small structures containing T cells that help the body fight infection and disease, and mesenteric lymph nodes typically prevent microbes from entering the rest of the body.
The researchers found that immunotherapy treatment dilated tiny blood vessels in mesenteric lymph nodes, assisting bacteria on their path to other lymph nodes and tumors.
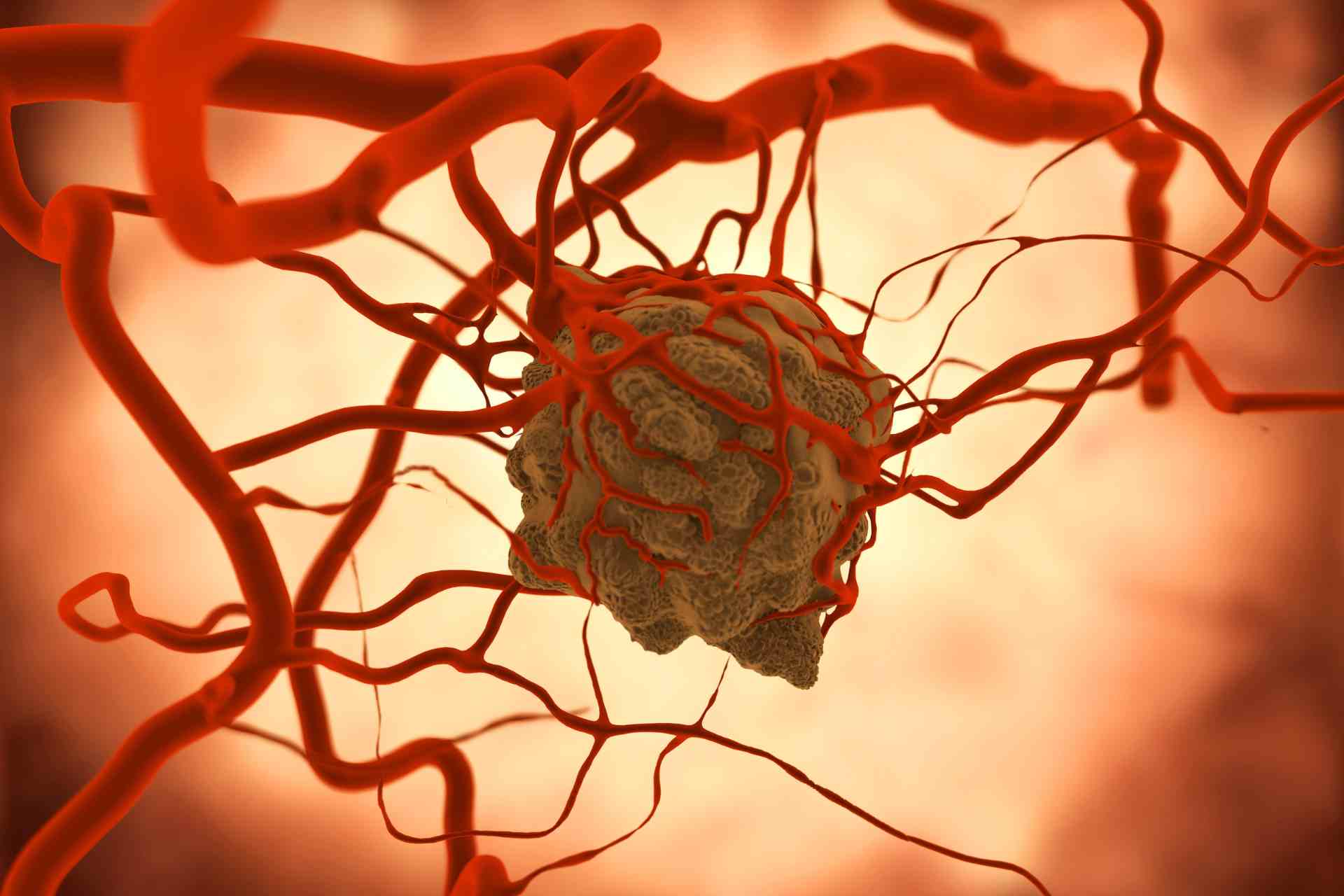
Further experiments showed that immunotherapy induced gut inflammation and activated a specific population of local immune cells called dendritic cells. Dendritic cells then carried beneficial gut bacteria past mesenteric lymph nodes, enabling the microbes to reach tumor-draining lymph nodes — sites where anti-tumor T cells are primed to tumor-specific antigens. Tumor-draining lymph nodes play key roles in immune responses against tumors.
Supercharged immunotherapy
Once inside tumor-draining lymph nodes, gut bacteria amplified the immune stimulation generated by immunotherapy treatment. They also boosted T cells’ anti-cancer activity, the researchers found.
Mice treated with antibiotics had fewer gut bacteria trafficking to tumors and a poorer response to immunotherapy. This result highlights the important role played by gut bacteria in increasing treatment efficacy.
“While the role of [dendritic cells] in anti-cancer immunity is well-established, our data provide an additional layer of insight in that gut bacteria-mediated anti-cancer immune effects may also be dependent on [dendritic cells] capacity to carry or traffic gut bacteria,” the researchers say.
Although it’s unclear whether the findings are generalizable to other tumor models, the authors add, “these principles could also apply to understanding whether and how gut microbiota modulate the efficacy of other cancer immunotherapies.”