• Microbial differences
• Altering the microbiota
What is already known on this topic
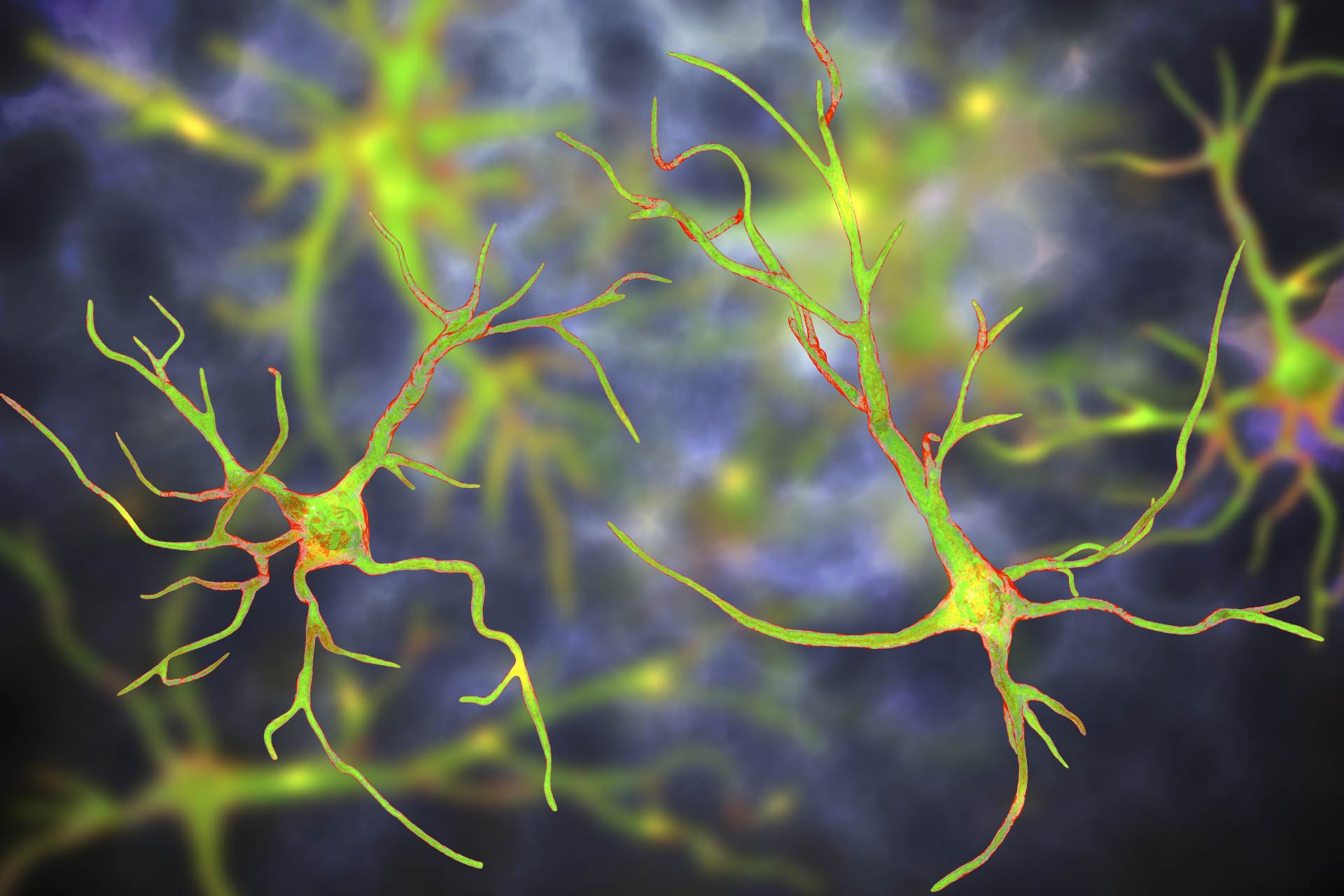
A mutation in the gene C9orf72 is the most common genetic variant that contributes to amyotrophic lateral sclerosis (ALS), a neurodegenerative disorder characterized by the progressive loss of neurons crucial for movement, speech, and cognition. However, only some individuals carrying the mutation develop ALS.What this research adds
By studying two population of mice with the same mutation in the gene C9orf72, researchers found that altering the animals’ gut microbiota with antibiotics or fecal transplants could prevent or improve disease symptoms.Conclusion
The findings suggest that microbial modulation of inflammation outside the brain could be responsible of how ALS symptoms manifest in mice that lack C9orf72.
In mice with a common genetic mutation linked to the neurodegenerative disorder amyotrophic lateral sclerosis, altering the gut microbiota could prevent or improve disease symptoms, a new study has found.
The results, published in Nature, could explain why only some individuals carrying the mutation develop amyotrophic lateral sclerosis, or ALS, which is characterized by the progressive loss of neurons crucial for movement, speech, and cognition.
To study one common mutation associated with ALS, Kevin Eggan at Harvard University and his colleagues created a mouse model of ALS in which animals have a mutation in the gene C9orf72. These mice had inflammation in the nervous system and the rest of the body, which led to a shortened lifespan.
However, the researchers noted that if the mice were housed at the Harvard University animal facility, they had a shorter lifespan and worse ALS symptoms than mice reared in an animal facility at the Broad Institute of MIT and Harvard. “These observations sparked our endeavor to understand what about the two different environments could be contributing to these different outcomes,” Eggan says.
Microbial differences
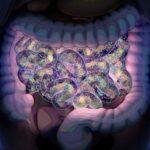
To understand the environmental differences between the two mice populations, the team compared the microbial profiles of the animals in the two facilities.
They found that bacteria such as Helicobacter, Pasteurella pneumotropica and Tritrichomonas muris were more common at the Harvard facility than at the Broad facility.
The rodents housed at the Broad facility had more diverse species of gut microbes and showed fewer inflammatory immune cells in their blood and spinal cord than did the animals kept at Harvard.
Altering the microbiota
To test whether the gut microbiota contributed to the inflammation seen in the mice at Harvard, the researchers administered antibiotics to the animals before the onset of inflammatory disease and then monitored the related symptoms for 200 days.
Antibiotic treatment prevented the induction of inflammatory molecules and reduced other signs of inflammation, including the presence of autoimmune antibodies and the enlargement of the spleen.
In mice treated with antibiotics, infiltration into the spinal cord by several types of immune cells was reduced compared to untreated animals. What’s more, inflammation in the Harvard mice was reduced if they received gut bacteria from animals reared at the Broad.
“Our results indicate that when C9orf72 function declines, the environment generally — and the gut microbiota specifically — become potent modifiers of whether autoimmunity, neural inflammation, motor deficits and premature mortality occur,” the researchers say.
Previous research has shown that the gut microbiota of people with ALS are different from those of healthy individuals. The new study provides further evidence that the gut microbiota plays an important role in brain health. The findings also suggest that microbial modulation of inflammation outside the brain could be responsible of how ALS symptoms manifest in mice that lack C9orf72, the researchers say.