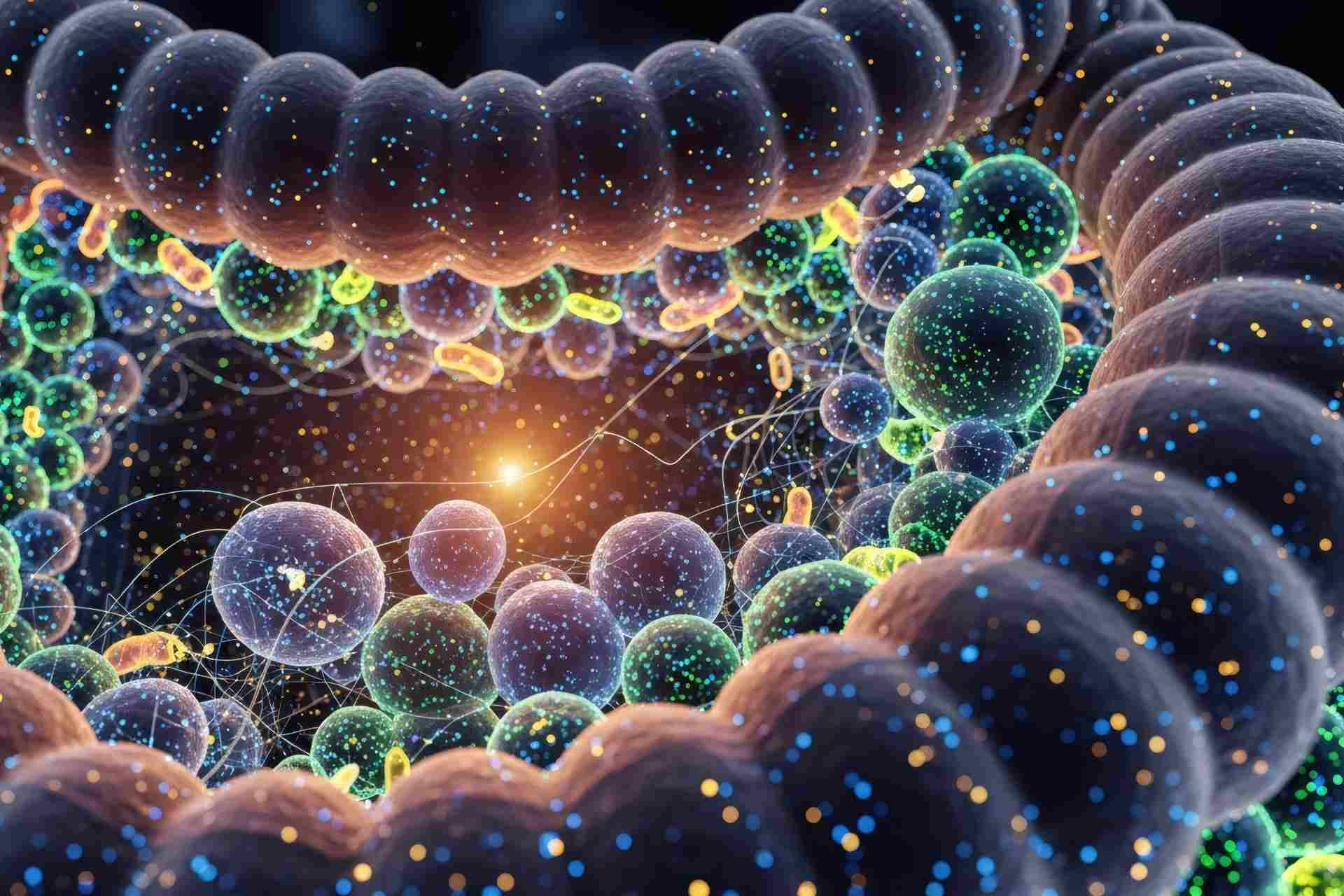
The gut hosts many helpful microbes, making it a good target for engineered bacterial therapies. Now, new research shows that engineered gut bacteria can be safely introduced and sustained in people for therapeutic functions.
The findings, published in Science, suggest that engineered bacteria can be used in gut therapies, but maintaining control over their colonization and genetic stability remains challenging.
Past approaches used short-lived bacteria, which were safe and worked well in animals, but they didn’t show strong results in people. Letting bacteria settle and grow in the gut might help reach more effective levels needed for treatment.
So, Weston Whitaker at Novome Biotechnologies in San Francisco, California, and his colleagues focused on using Phocaeicola vulgatus, a common gut microbe in Western populations, to treat enteric hyperoxaluria—a condition where the body absorbs too much dietary oxalate, causing kidney stones.
The same team had previously engineered P. vulgatus to digest porphyran—a rare seaweed sugar—giving it a unique advantage to colonize the gut.
Engineered bacteria
Enteric hyperoxaluria can happen when beneficial gut bacteria that normally break down oxalate are missing, for example due to antibiotic treatments. The researchers engineered P. vulgatus to break down oxalate by inserting specific genes that convert it into a harmless compound called formate.
In rats, the engineered microbe reduced oxalate levels in urine, especially when paired with porphyran. To ensure safety and control, the team also made the bacteria dependent on porphyran for survival, which means the microbes can be removed from the gut simply by removing porphyran.
In a clinical trial, the team tested the engineered bacterium in healthy volunteers. Colonization success improved when participants took a drug that helps protect the stomach, and higher porphyran doses led to more bacteria in the gut, the researchers found.
Therapeutic activities
After stopping porphyran, the engineered P. vulgatus was cleared in most people, but in a few individuals, it persisted due to rare genetic mutations that let it grow without porphyran. Though these cases caused only mild, temporary side effects, the team engineered a new version of the microbe that makes it much harder for mutations to let it grow without porphyran. In lab and animal tests, this approach ensured the bacteria disappeared when porphyran was removed, but some low-level persistence still occurred.
In people with enteric hyperoxaluria, the microbe did not colonize the gut as well as it did in healthy volunteers. And in some people, the bacteria lost key functions through gene exchange with native microbes, reducing treatment durability.
The approach may require improvements to boost its effectiveness, the researchers say. Regardless, they add, the findings “offer a tool to deliver defined therapeutic activities to the human colon.”