-
What is already known on this topic
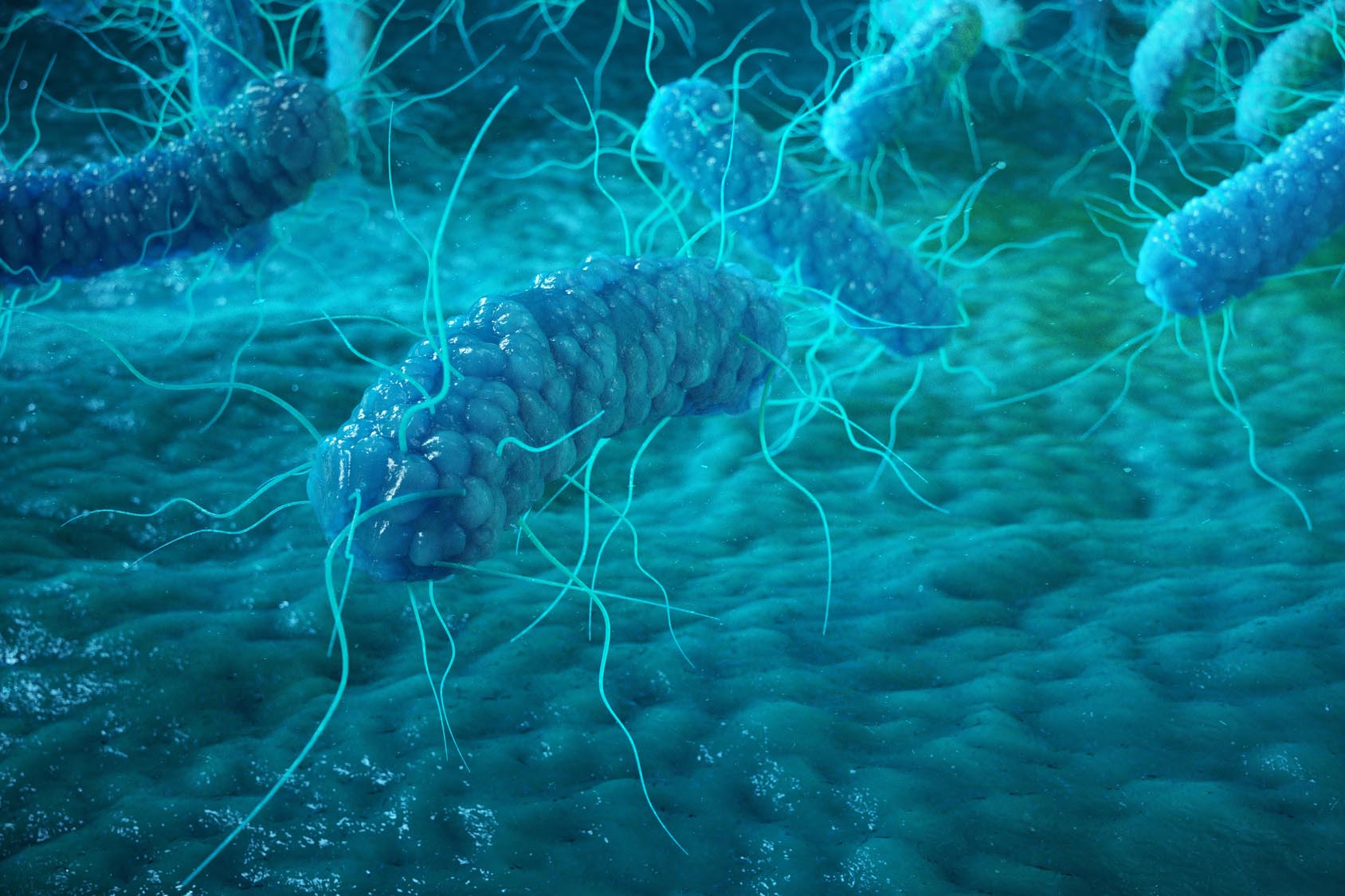
Clostridioides difficile (previously known as Clostridium difficile) is an opportunistic pathogen that causes severe and sometimes life-threatening diarrhea. Disruptions of the gut microbiota structure can create a favorable environment for C. difficile, but the metabolic factors that contribute to the development of C. difficile infection remain unclear. -
What this research adds
In mice, the disruption of gut microbiota allows C. difficile to thrive by increasing the levels of the amino acid proline. The study also looked at patients with diarrhea and identified risk factors that might predict gut microbial dysbiosis and thus why some people may be more susceptible to C. difficile infection. -
Conclusions
Identifying factors that contribute to C. difficile infection could lead to new therapeutic approaches.
In mice, an altered gut microbiota composition leads to an increase in certain amino acids, particularly proline, which is used as a food source by the opportunistic pathogen C. difficile. This gives the microbe a competitive advantage and favors the development of C. difficile infection, new research has found. The study, led by Eric Battaglioli of the Mayo Clinic in Rochester, Minnesota, was published in Science Translational Medicine.
C. difficile can cause severe and sometimes life-threatening diarrhea. Alterations of the microbial gut community, for example after antibiotic intake, can reduce the gut microbial diversity as well as the production of inhibitory metabolites. This creates a favorable environment for C. difficile, but the metabolic factors that contribute to the development of C. difficile infection are still unclear. To characterize these factors, the researchers conducted experiments in both humans and mice.
Some people with diarrhea have a different gut microbiota from that of healthy people
The team analyzed the gut microbial composition of 115 people with diarrhea. The gut microbiota could be divided in two groups: a healthy-like microbiota, which was similar to that of healthy people, and a dysbiotic microbiota, which was similar to that of people with C. difficile infection.
Five factors predicted dysbiosis in people with diarrhea: antibiotic intake within the previous 3 weeks, immunosuppression, current or recent hospitalization, and prior C. difficile infection.
A dysbiotic gut microbiota is more susceptible to C. difficile infection than a healthy-like one.
To test the effects of dysbiosis on the susceptibility to C. difficile infection, the researchers transferred the gut microbiota from two dysbiotic and two healthy-like people into germ-free mice. Then, they gave C. difficile to the rodents. Compared to mice that received healthy-like gut microbiota, those that received dysbiotic microbiota showed:
- significantly higher loads of C. difficile in stool
- softer stool consistency
- increased amounts of C. difficile toxin B in stool
- increased inflammation
- higher levels of cytokines associated with C. difficile infection in the colon
A dysbiotic gut microbiota is characterized by an altered metabolic state
Next, the team used transcriptomics, metabolomics, and nuclear magnetic resonance to analyze the stool of dysbiotic and healthy-like mice and define the factors that favored C. difficile infection. Compared to healthy-like mice, dysbiotic mice showed:
- reduced expression of several genes related to amino acid uptake and metabolism as well as short-chain fatty acids and secondary bile acids production
- increased levels of 12 amino acids, particularly proline
Previous studies have shown that amino acids modulate toxin production and support C. difficile infection in antibiotic-treated mice. So the team set out to assess C. difficile growth in a medium with decreasing amino acid concentrations. The pathogen grew better at higher amino acid concentrations, which suggests that amino acid availability gives it a competitive advantage under permissive conditions, such as low levels of secondary bile acids.
The ability to use proline gives C. difficile a competitive advantage in dysbiotic mice
C. difficile has been shown to be able to use the amino acid proline as its only energy source. Indeed, the researchers found that both dysbiotic and healthy-like mice had a higher expression of prdA, an enzyme that contributes to proline metabolism. However, in healthy-like mice, three commensal bacterial species expressed prdA, whereas in dysbiotic mice, only C. difficile expressed it.
What’s more, mice fed a diet that lacked proline had a five-fold lower C. difficile load in their gut compared to mice fed a normal diet.
Fecal transplant reduces free proline and susceptibility to C. difficile infection in dysbiotic mice
Finally, to determine whether fecal microbiota transplant could reduce C. difficile susceptibility in dysbiotic mice, the team transferred the gut microbiota of a healthy person to dysbiotic and healthy-like mice.
While the gut microbiota of healthy-like mice was unchanged after the transplant, that of dysbiotic mice increased in microbial richness. Dysbiotic mice became resistant to C. difficile infection, showing no sign of gut inflammation and no C. difficile in stool. In these mice, the fecal transplant also resulted in a significant decrease in free proline.
In summary, the study shows that the metabolic environment generated by gut microbial dysbiosis can modulate the susceptibility to C. difficile infection. The study also pinpointed potential factors associated with dysbiosis and C. difficile infection, which could lead to new prevention and treatment strategies. However, further research is needed to validate these factors in different patient cohorts.