What is already known on this topic
Patients with Parkinson’s disease (PD) frequently have gastrointestinal symptoms, and recent studies reported an association between changes in gut microbiota composition and PD.What this research adds
Using gene sequencing and analyzing bacterial metabolic networks, the researchers have conducted a meta-analysis of gut dysbiosis in PD using 5 datasets of different countries.Conclusion
This study published in Movement Disorders has identified an increased abundance of the genus Akkermansia that might be responsible for pathological alterations of intestine mucosa in PD patients.
Parkinson’s disease (PD) is the second most common neurodegenerative disease, affecting millions of people worldwide. Characteristic features of PD include symptoms such as tremors and difficulty walking, aggregation of a protein called alpha-synuclein within cells in the brain and in non-neuronal tissues, including the olfactory bulb, skin, salivary glands, and gut. Moreover, 75% of people with PD present gastrointestinal abnormalities, including constipation. Various studies on animal models and humans have previously suggested a functional link between bacteria in the intestines and PD.
Here, using 16S ribosomal RNA gene sequencing and analyzing datasets from the United States, Finland, Russia, Germany, and Japan, researchers demonstrate a change in the composition of gut bacteria in PD across countries. In particular, to identify differences in bacterial taxa in PD, the team analyzed fecal samples from 223 PD patients and 137 controls, and conducted a meta-analysis of the Japanese dataset they generated and of four datasets already available from the other countries. Subjects who took antibiotics 30 days before the study have been excluded.
The team found that:
- Certain bacteria were increased in PD, including genera Akkermansia and Catabacter, as well as families Akkermansiaceae.
- Other taxa were found to be decreased in PD, such as genera Roseburia, Faecalibacterium, and Lachnospiraceae ND3007 group.
- Increased genus Akkermansia and decreased genera Roseburia and Faecalibacterium were frequently observed across countries.
Importantly, the researchers compared six features between PD patients and controls, that are known to influence the gut bacterial population, such as age, sex, body mass index (BMI), constipation, proton pump inhibitor, H2 blocker and Catechol-O-methyl transferase (COMT) inhibitor used for the treatment of PD.
All covariates significantly influenced gut microbiome composition across PD patients, therefore the team investigated how confounding factors influenced bacterial taxa abundance, and found that:
- Fifteen genera and four families were changed in PD after adjusting for constipation, BMI, sex, age, and COMT inhibitor intake.
- COMT inhibitor intake markedly increased family Lactobacillaceae and decreased the genus Lachnospira.
- Constipation affected three genera (Faecalibacterium, Lachnospiraceae UCG-004, and Lachnospiraceae ND3007 group) and two families (Family XIII and Rikenellaceae).
- Sex also influenced bacterial composition in PD. AD3011 group was increased in males.
- Other genera were affected by age (Family XIII AD3011 group and Blautia) and one family too (Christensenellaceae).
After adjusting for confounding factors, network analysis of bacteria confirmed that Akkermansia and Christensenellaceae R-7 group were significantly increased in PD, while other genera such as Faecalibacterium, Roseburia, and Fusicatenibacter were reduced.
Using KEGG (Kyoto Encyclopedia of Genes and Genomes), a collection of databases for bioinformatics research, the team investigated on PD metabolomics, revealing that 19 pathways were upregulated, including butanoate and propionate metabolisms, and three pathways were downregulated.
The team then performed a meta-analysis of the datasets, founding 18 genera and seven families significantly and homogenously changed across five countries. Adjustment for possible confounding factors further confirmed that genera Akkermansia and family Akkermansiaceae were increased, and genera Roseburia and Faecalibacterium were decreased. Moreover, the genus Akkermansia was increased with the progression of PD, whereas genera Faecalibacterium and Roseburia were decreased.
Previous studies have reported that variation in gut microbiota in PD might be accompanied by altered concentrations of short-chain fatty acids (SCFA), one main metabolic product of gut bacteria. Therefore, the team suggested that decreased abundance of the genera Roseburia and Faecalibacterium may account for decreased intestinal SCFAs, which leads to neuroinflammation in PD.
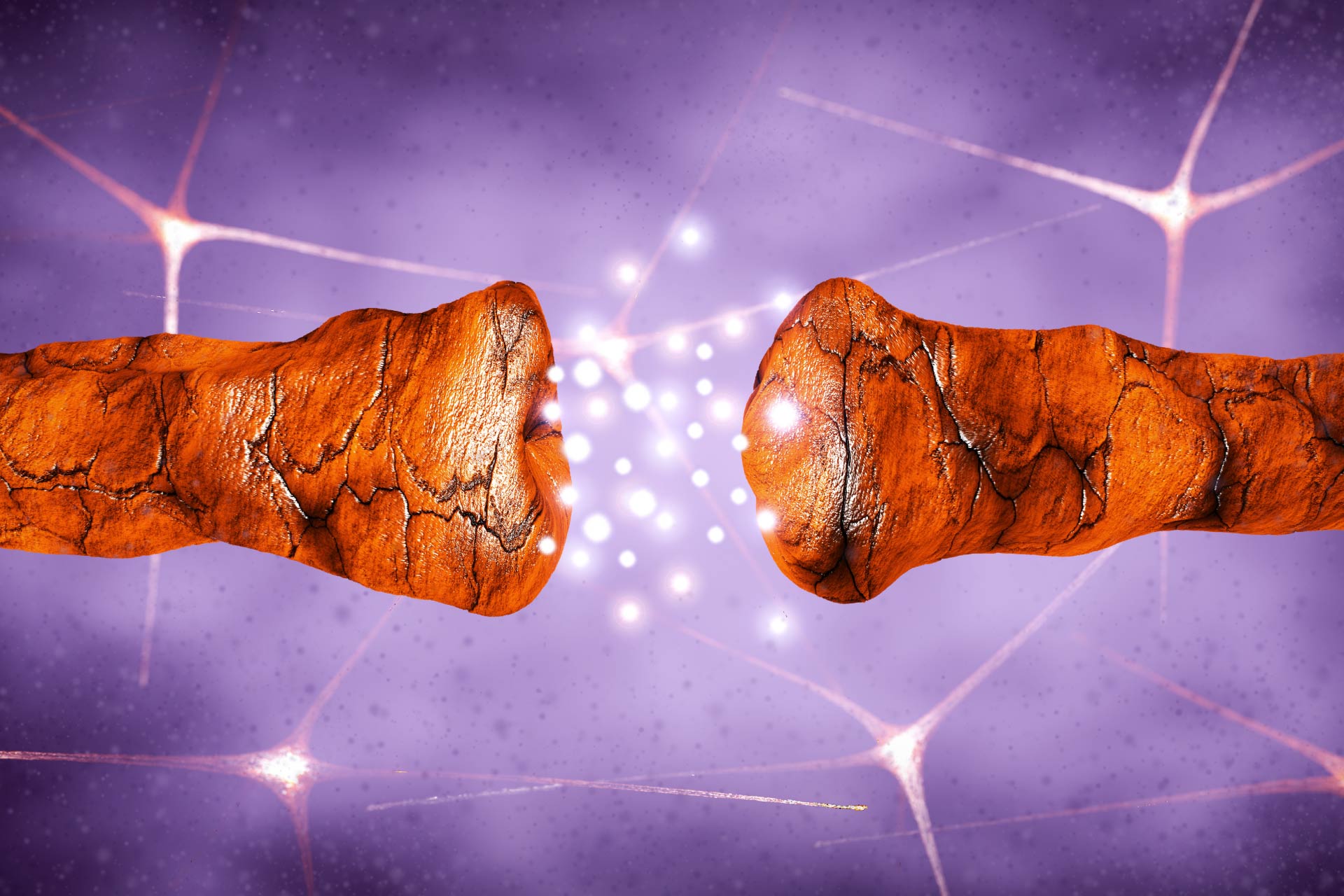
Furthermore, an increased abundance of Akkermansia muciniphila, which degrades the mucus layer of the gut, could affect intestinal permeability in PD, exposing intestinal neural plexus directly to damaging factors, such as oxidative stress or pesticide and herbicides, possibly determining abnormal aggregation of α-synuclein fibrils in the intestine.
In summary, the team has identified bacterial taxa that are significantly changed in PD, across different countries, and when adjusted for confounding factors. As the team underlined, plenty of observations in humans suggest that abnormal accumulation of α-synuclein fibrils could start from the intestine and ascends to the midbrain affecting the nervous system. Therefore, gut bacteria could actively contribute to the hallmark of PD, and patients with more changes in certain taxa may have a more accelerated disease progression. Further studies are required to prove whether the changes in these taxa are the consequences or causes of the progression of PD.