• HIV treatment
• Immune recovery
What is already known on this topic
Increased activation of specific immune cells and raised markers of inflammation are associated with negative health outcomes during ‘combination antiretroviral therapy’ (cART), a combination of drugs used to keep HIV infections under control. Scientists have known that microbial translocation into the blood can cause inflammation and immune reconstitution in people infected with HIV, but the underlying mechanisms remain unclear.What this research adds
By following HIV-infected individuals for two years after cART initiation, researchers have detected changes in translocated constituents of the microbiota. Over the course of the first year, increased numbers of immune cells called CD4 T cell were associated with high levels of Serratia bacteria and pro-inflammatory immune molecules, which drive inflammation and a first wave of immune reconstitution. In the second year, reduced levels of Serratia and of inflammatory molecules were associated with immune reconstitution and CD4 T cell recovery. CD4 T cell recovery is a key measure of clinical outcome.Conclusion
The findings suggest that the microbiota plays a key role in the resolution of inflammation and the recovery of immunity after HIV treatment. Targeting specific components of the microbiota at different stages during cART therapy could help to reduce disease and death in people infected with HIV.
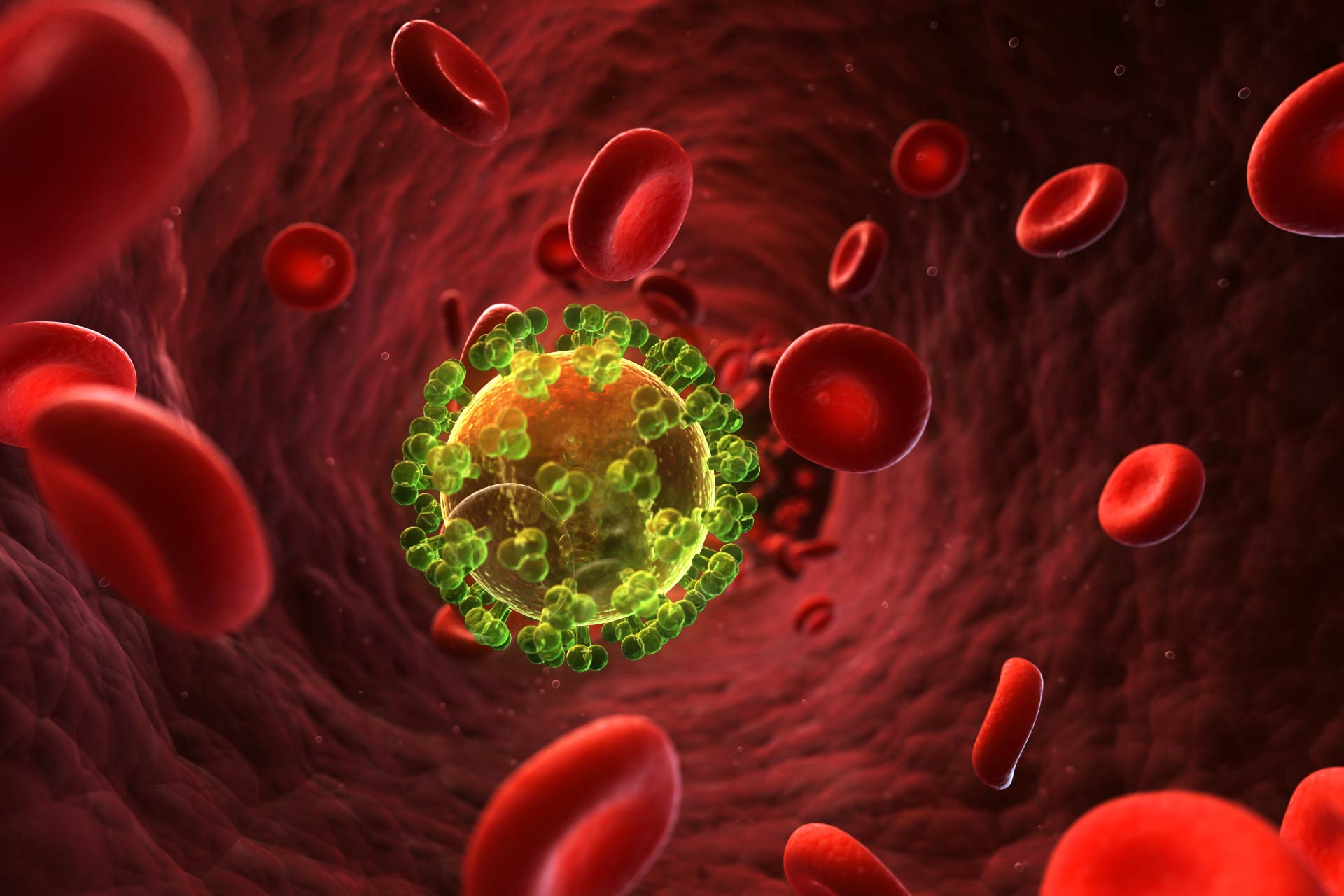
Despite advances in the treatment of HIV infections, mortality remains high in people treated for HIV infections compared to uninfected individuals. Now, researchers have found that translocated gut microbes in the blood of HIV-infected people treated with combined antiretroviral therapy results in two waves of immune recovery.
The findings, published in Cell, suggest that the microbiota plays a key role in the resolution of inflammation and the recovery of immunity after HIV treatment. Targeting specific components of the microbiota at different stages during HIV treatment could help to reduce disease and death in infected individuals, the researchers say.
Increased activation of specific immune cells and raised markers of inflammation are associated with long-term disease and mortality during ‘combination antiretroviral therapy’ (cART), a combination of drugs used to keep HIV infections under control. Scientists have known that microbial translocation into the blood can cause inflammation and immune reconstitution in treated and untreated HIV infection, but the underlying mechanisms remain unclear.
A team of researchers led by Daniel Douek at the US National Institutes of Health set out to analyze how gut microbes interact with components of the immune system during cART.
HIV treatment
The researchers followed 11 HIV-infected individuals for two years after cART initiation. By day 7, the levels of HIV in the individuals’ blood decreased an average 100-fold and complete virus suppression was achieved after 3 to 4 months in most participants, the team found.
At the beginning of therapy, all participants had elevated levels of immune markers compared to uninfected people, which suggests an altered pattern of inflammation. Pro-inflammatory immune molecules increased after cART initiation up to month 12, and declined by month 24.
To measure microbial levels in a person’s circulation, the researchers sequenced DNA and RNA fragments found in the participants’ blood at the beginning of cART therapy and after 3, 4, 9, 12, and 24 months. They found that circulating microbial nucleic acids were mostly belonging to Proteobacteria and were associated with increased inflammation. The levels of Proteobacteria were high within the first year following cART, whereas Actinobacteria, Bacteroidetes, and Firmicutes were higher at months 4 and 24.
Immune recovery
The researchers found that the genus Serratia was the most abundant among the Proteobacteria. Over the course of the first year, increased numbers of immune cells called CD4 T cell were associated with high levels of Serratia bacteria and pro-inflammatory immune molecules, which drive inflammation and a first wave of immune reconstitution.
In the second year, reduced levels of Serratia and of inflammatory molecules were associated with immune reconstitution and CD4 T cell recovery. CD4 T cell recovery is a key measure of clinical outcome.
The results led the researchers to propose a model in which the initial inflammatory response to Serratia results in T cell differentiation and repair of the gut barrier. As the immunity is restored, the composition of the gut microbiota changes, triggering T cell differentiation programs. This promotes further CD4 T cell recovery over the course of the second year after cART initiation.