What is already known
Immune checkpoint inhibitors — a class of drugs that help the immune system recognize and attack cancer cells — have revolutionized cancer treatment. But despite success in some cancers, many patients develop resistance. Previous studies have suggested that fecal microbiota transplantation from responsive patients can boost treatment efficacy, but which gut bacteria play a causal role in this process remains unknown.
What this research adds
Researchers transferred gut bacteria from donors who had previously benefited from anti-PD-1 therapy to 13 recipients with advanced gastrointestinal cancer who had not responded to such treatments. After fecal microbiota transplantation, six patients showed improved responses to immunotherapy. The team identified specific bacterial strains that influenced the effectiveness of the treatment.
Conclusions
The findings support the idea that the gut microbiota modulates immune responses, suggesting new avenues for cancer treatment.
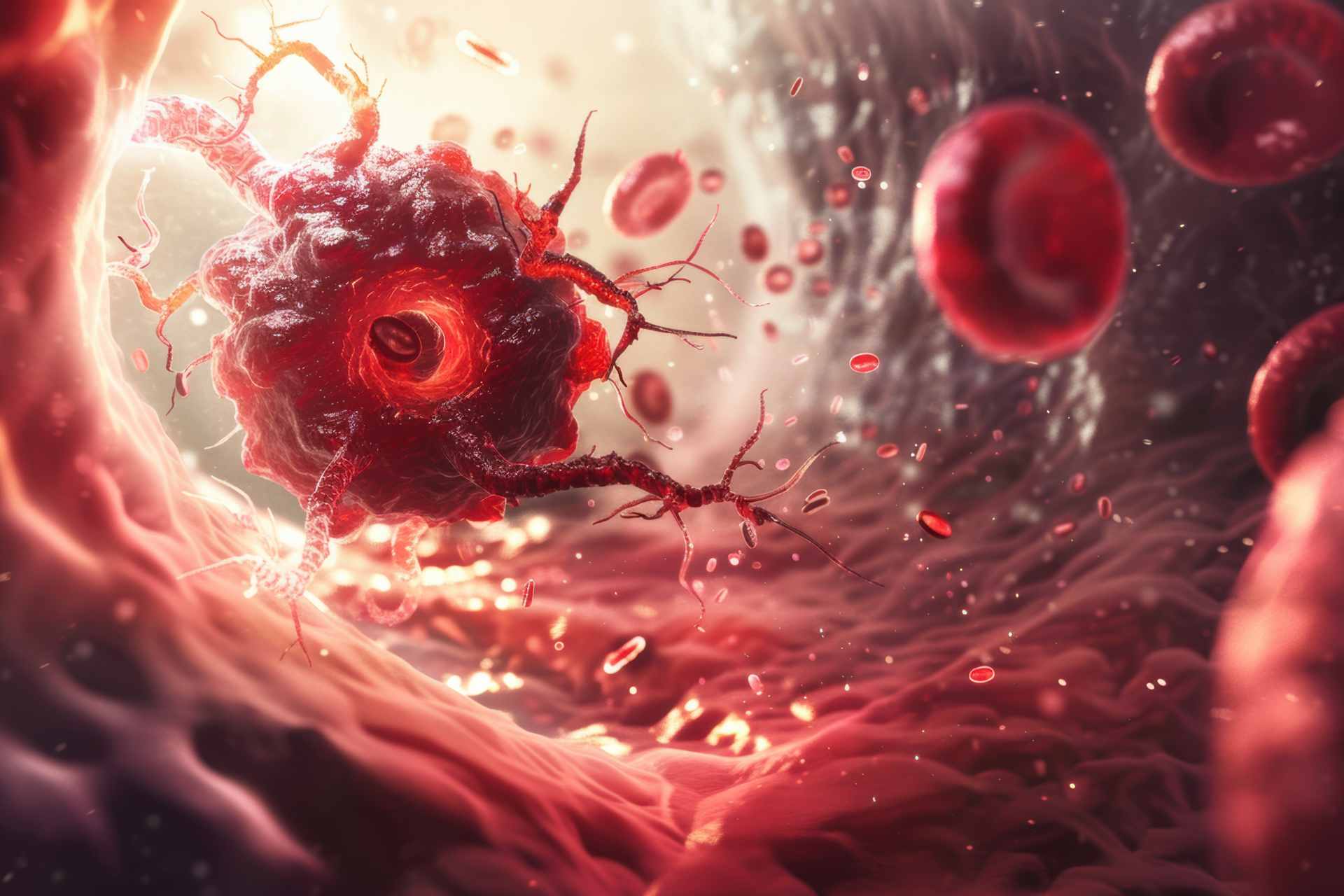
Immune checkpoint inhibitors — a class of drugs that help the immune system recognize and attack cancer cells — have revolutionized cancer treatment. But despite success in some cancers, many patients develop resistance. Now, a small clinical trial shows that gut bacteria from donors who had previously benefited from immune checkpoint inhibitors can boost the effectiveness of immunotherapy in people with advanced gastrointestinal cancer who had not responded to such treatments.
The findings, published in Cell Host & Microbe, support the idea that the gut microbiota modulates immune responses, suggesting new avenues for cancer treatment.
“This research highlights the complex interplay between beneficial and detrimental bacteria within the gut microbiota in determining treatment outcomes,” says study co-author Hansoo Park at the Gwangju Institute of Science and Technology in Gwangju, South Korea. “While the connection between gut microbiota and immune response to cancer therapy has been a growing area of interest, our study provides concrete evidence and new avenues for improving treatment outcomes in a broader range of cancers.”
Previous research has suggested that transferring stool from responsive patients into the gut of people who did not respond to immunotherapy can boost treatment efficacy in some skin cancers. However, it is unclear how this procedure — known as fecal microbiota transplantation — can help overcome resistance to a class of immune checkpoint inhibitors called anti-PD-1 inhibitors in people with other types of cancer. What’s more, which gut bacteria can boost treatment effectiveness remains unknown.
To address these questions, Park and his team administered a fecal microbiota transplant to 13 people with advanced gastrointestinal cancer who had not responded to anti-PD-1 inhibitors.
Boosting treatment efficacy
All study participants had metastatic cancers that were resistant to the anti-PD-1 drug nivolumab. Four people had gastric cancer, five had esophageal cancer, and four had hepatocellular carcinoma — a type of cancer that originates from the main type of liver cells.
The stool donors had the same types of cancer and responded to treatment with nivolumab or another anti-PD-1 drug called pembrolizumab. After recipients took antibiotics to reduce their existing gut microbiota, they received the fecal microbiota transplantation through a colonoscopy procedure.
“One of the most surprising results was from a hepatocellular carcinoma patient who initially showed no response to the first [fecal microbiota transplantation] and continued to experience cancer progression,” says study co-author Sook Ryun Park. “However, after switching the donor for the second [fecal microbiota transplantation], the patient exhibited remarkable tumor shrinkage.”
Targeting the microbiota
Next, the researchers set out to investigate which bacteria were more likely to determine the success of a fecal microbiota transplant combined with checkpoint inhibitors. They found that a bacterial strain called Prevotella merdae Immunoactis, which had not been previously described, boosted the effectiveness of fecal microbiota transplantation. Two other bacterial strains, Lactobacillus salivarius and Bacteroides plebeius, reduced treatment efficacy.
The researchers now plan to continue studying these and other strains to develop strategies that target the gut microbiota to improve responses to cancer immunotherapy. “By examining the complex interactions within the microbiome, we hope to identify optimal microbial communities that can be used to enhance cancer treatment outcomes,” Hansoo Park says. “This comprehensive approach will help us understand how the microbial ecosystem as a whole contributes to therapeutic success.”
However, the authors caution that fecal microbiota transplantations carry the risk of transmitting harmful microbes. The procedure also lacks standardized protocols and regulatory guidelines. “Developing efficient and cost-effective methods for production and distribution is necessary for widespread adoption,” Sook Ryun Park says. “Addressing these challenges through comprehensive research and careful planning will be essential for integrating [fecal microbiota transplantation] into the standard of care for cancer treatment.”