• Combined effects
• Enhancing treatment
What is already known on this topic
Although colon cancer is one of the leading causes of death from cancer worldwide, this type of tumor has not benefited from advances in immunotherapy and precision medicine. The drug oxaliplatin, which triggers the programmed death of cells in the terminal part of the intestine, called ileum, remains the only treatment of this type of tumor. However, the prognosis of colon cancer is also influenced by tumor-infiltrating immune cells, including follicular helper T (TFH) cells, which can be influenced by the gut microbiota.What this research adds
In both mice and people with colon cancer, treatment with oxaliplatin elicited more beneficial effects if cells in the terminal part of the intestine underwent programmed cell death. The prognosis of rodents and people with this type of cancer improved if the ileal microbiota was rich in bacteria such as Bacteroides fragilis or Erysipeloclostridium ramosum.Conclusion
The results show the importance of the ileum and its microbiota in the response to cancer treatment. The findings also open up new avenues for anti-cancer approaches, including molecules that induce cell death of ileal cells as well as bacterial species that trigger immune responses against colon cancer antigens.
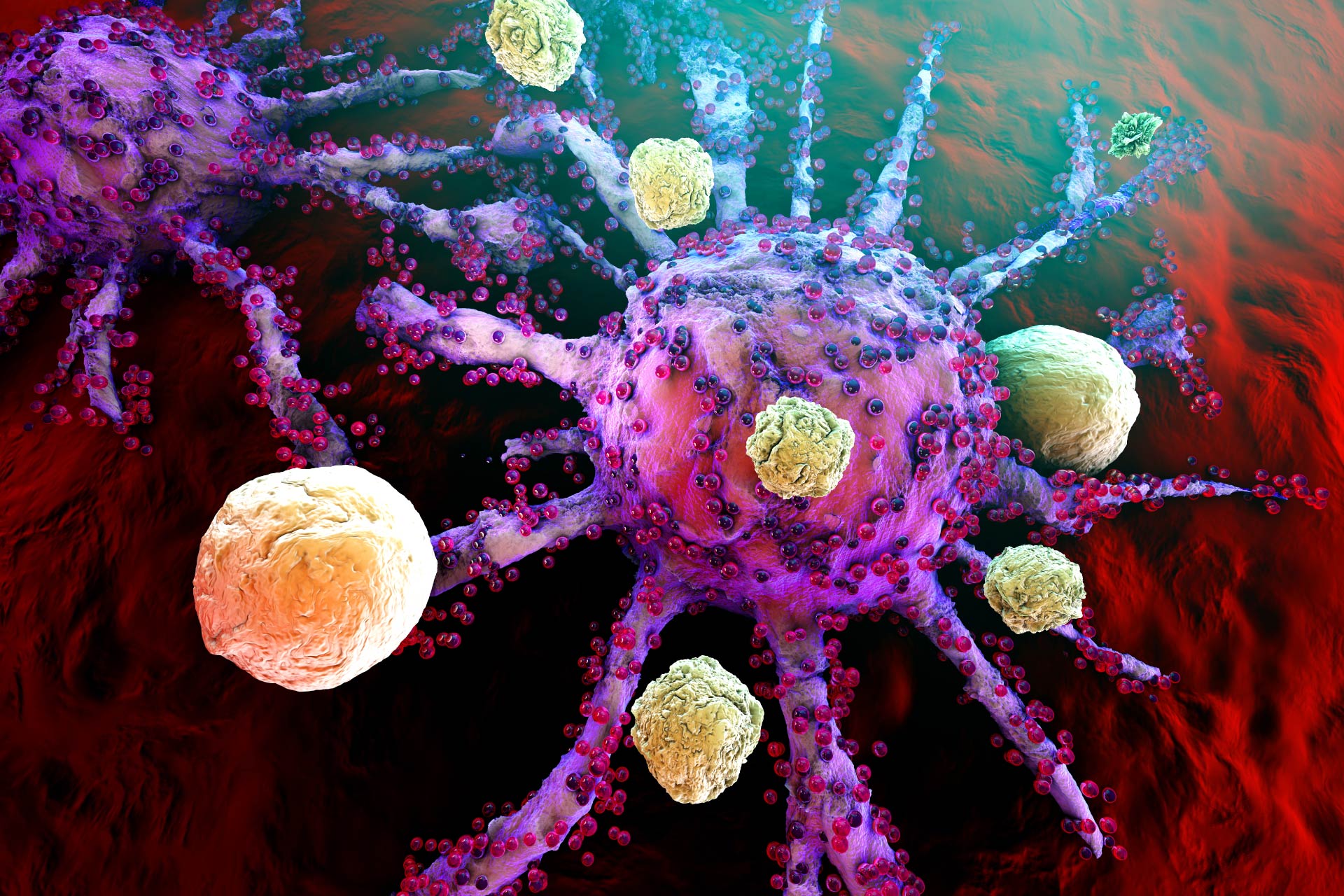
Colon cancer is one of the leading causes of death from cancer worldwide. Now, researchers have found that the gut microbiota and the death of intestinal cells caused by chemotherapy can enhance the immune response of people with colon cancer.
The findings, published in Nature Medicine, could help to better understand why some people respond well to cancer treatment whereas others don’t.
Unlike other types of cancer, colon cancer has not benefited from advances in immunotherapy and precision medicine. The drug oxaliplatin, which triggers the programmed death of cells in the terminal part of the intestine, remains the only treatment of this type of tumor. However, the prognosis of colon cancer is also influenced by tumor-infiltrating immune cells, including follicular helper T (TFH) cells.
To understand whether gut microbes contribute to TFH cell-driven responses, Laurence Zitvogel at the Gustave Roussy Cancer Campus and her colleagues analyzed the conditions that generate a successful response to chemotherapy.
Combined effects
In both mice and people with colon cancer, the researchers observed that treatment with oxaliplatin elicited more beneficial effects if cells in the terminal part of the intestine, or ileum, underwent programmed cell death. What’s more, the prognosis of rodents and people with this type of cancer improved if the ileal microbiota was rich in bacteria such as Bacteroides fragilis or Erysipeloclostridium ramosum.
These two conditions are associated with TFH cell activation, which in turn triggers the activity of other immune cells, increasing the host immune response against cancer. By contrast, an intestinal flora enriched in bacterial species such as Fusobacterium nucleatum was associated with decreased immune system responses and a poor prognosis.
The team also found that the efficacy of oxaliplatin treatment was reduced in mice whose microbiota was suppressed by antibiotic treatment.
Enhancing treatment
The researchers showed that in mice that do not normally respond to immunotherapy, adding bacteria such as B. fragilis or E. ramosum reinstates the benefits of immunotherapy treatment.
Taken together, the results highlight the importance of the ileum and its microbiota in the response to cancer treatment.
The findings also open up new avenues for anti-cancer approaches, including molecules that induce cell death of ileal cells as well as bacterial species that trigger immune responses against colon cancer antigens, the researchers say.