• Metabolism matters
• Stimulating memory cells
What is already known on this topic
Several studies have uncovered links between gut microbes and immune cells, but the exact microbial signals that trigger the immune system remain unclear.What this research adds
Both the gut microbiota and microbiota-derived metabolites can influence the ability of killer immune cells to differentiate into memory immune cells. In the absence of microbiota, killer cells failed to give rise to memory cells.Conclusions
The findings reveal a role for the microbiota in the survival of activated immune cells as memory cells, potentially through metabolic changes in immune cells in response to microbial metabolites.
The bacteria living in the gut could boost the activity of immune cells, a study done in mice finds. The results, published in the journal Immunity, are in line with previous research that uncovered links between gut microbes and immune cells.
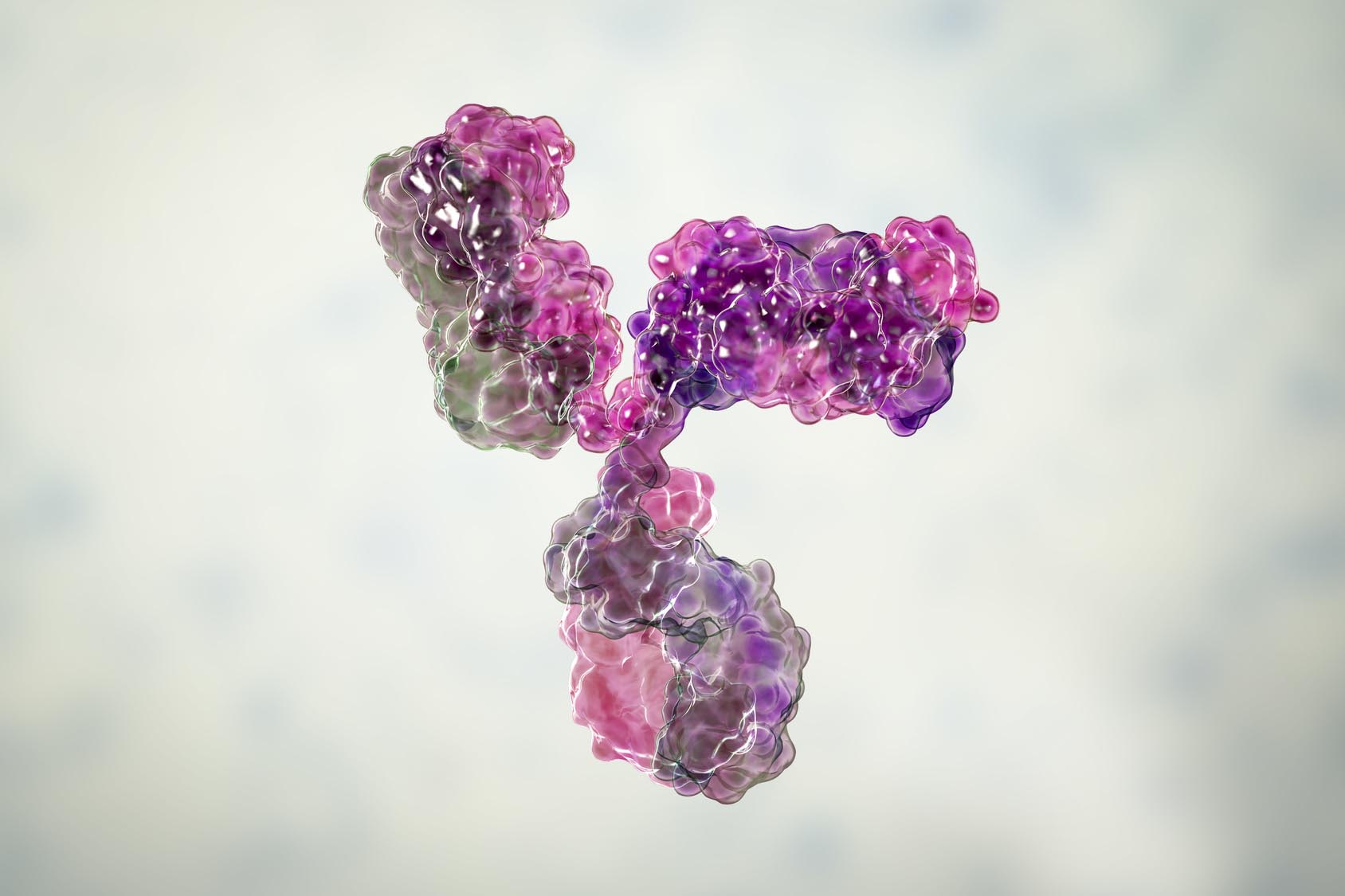
However, little is known about the exact microbial signals that trigger the immune system, so Annabell Bachem at the University of Melbourne and her colleagues set out to examine whether the gut microbiota and microbiota-derived metabolites such as short-chain fatty acids (SCFAs) could influence the ability of killer immune cells to differentiate into memory immune cells.
Stimulating memory cells
To assess whether activated CD8+ T cells require microbiota-derived signals to give rise to memory cells, the team transferred activated immune cells into specific-pathogen-free and germ free mice. In germ free mice, which completely lack the microbiota, killer cells failed to give rise to memory cells.
Because gut microbes produce many metabolites that influence and regulate the physiology of the host, the researchers tested whether increasing the levels of SCFAs in mice could enhance the memory capacity of activated CD8+ T cells. To do so, they fed mice a high-fiber diet, which results in a 100-fold increase in circulating butyrate levels.
Elevating the levels of SCFAs such as butyrate boosted the ability of killer cells tosurvive and form memory cells.
Metabolism matters
To explore how SCFAs influence the activity of immune cells, the researchers exposed activated CD8+ T cells to different SCFAs. The microbiota-derived metabolites promoted memory differentiation of activated immune cells by modifying the metabolism of the cells.
In particular, SCFAs helped killer immune cells to rely less on sugar and instead burn fats. This switch is critical for their long-term survival, as cells that only rely on burning glucose fail to survive, the scientists say.
Although a high-fiber diet has a dramatic effect on the microbiota-mediated activity of immune cells, it’s unclear whether only the gut microbiota is able to influence the survival of memory cells or whether the microbiota of other body sites such as the skin and lungs may also play a role.
The researchers hope that their study could lead to new drugs that improve the effectiveness of cancer immunotherapy, a type of treatment that aims at boosting the body’s own immune system to fight off tumors.