• The gut-brain axis
• Influencing disease
What is already known on this topic
Alzheimer’s disease (AD), characterized by protein tangles that cause nerve cells to die, is the most common neurodegenerative disease. Although aging is the major risk factor of AD, studies of the intestinal flora of individuals with the disorder have shown that their bacterial communities differ from those of healthy people. But the mechanisms behind these links have remained unclear.What this research adds
Working in mouse models of AD, researchers showed that as animals develop the first symptoms of AD, there are also changes in the intestinal flora associated with increased activity of a specific signaling pathway. Treating mice with antibiotics to reset the gut microbiota or with drugs to block the signaling activity attenuated the accumulation of plaques in the brain, improving cognitive functions.Conclusion
Although more studies are needed to assess the extent to which the findings can be transferred to people, the results suggest that an optimized diet or nutritional supplements could help to counteract the development of AD or slow down its progression.
“Good” bacteria in the gut seem to protect against an Alzheimer’s-like disease in mice, a new study has found.
The findings, published in Science Advances, suggest that optimizing the intestinal flora through a healthy diet or food supplements can inhibit the development of Alzheimer’s disease (AD), the most common neurodegenerative disease.
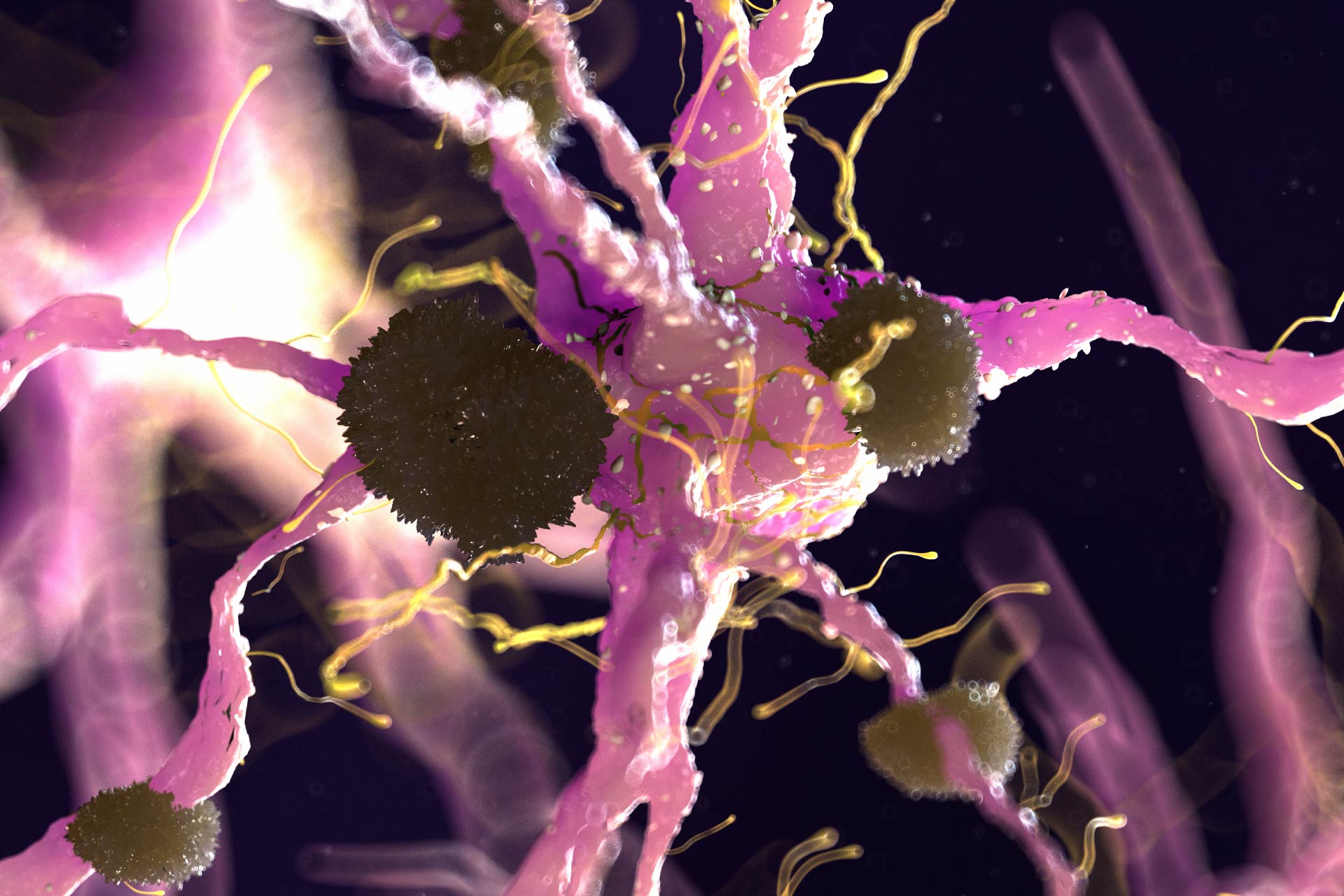
AD is characterized by protein tangles that accumulate in the brain, causing nerve cells to die. Although aging is the major risk factor, studies of the intestinal flora of people with AD have shown that their bacterial communities differ from those of healthy people. But the mechanisms behind these links have remained unclear.
To assess how an imbalance of bacteria in the gut is linked to AD, a team of researchers led by Ashfaqul Alam at the University of Kentucky and Keqiang Ye at Emory University analyzed genetically engineered mice that develop AD at an age of around twelve months.
The gut-brain axis
The researchers first investigated whether the gut microbiota of the mouse models of AD differs from that of healthy mice. The composition of the bacterial communities in the gut differed little in mice up to six months of age. But as mice developed the first symptoms of AD, the researcher observed alterations in the animals’ intestinal flora—a condition known as gut dysbiosis. In particular, mice with AD had more pro-inflammatory bacteria and less anti-inflammatory bacteria in their guts than healthy rodents.
The researchers found that the imbalance in the intestinal flora of the mice with AS was linked to an increased activity of a signaling pathway called C/EBPβ/AEP, which is known to trigger the formation of protein tangles in the brain, leading to the progression of AD.
The team also showed that when young mice prone to developing AD were housed with older mice with the condition, the young rodents were exposed to the older animals’ altered gut microbiota, and they developed AD faster than their siblings that were housed with healthy mice.
Influencing disease
Giving mice antibiotics to reset the gut microbiota attenuated the accumulation of plaques in the brain, improving cognitive functions. Treating the animals with drugs that block the C/EBPβ/AEP signaling pathway also alleviated the development of AD.
“Our findings support the hypothesis that C/EBPβ/AEP signaling is activated by gut dysbiosis, implicated in AD pathologies in the gut,” the researchers say.
Although more studies are needed to investigate the extent to which the findings can be transferred to people, the results suggest that an optimized diet or nutritional supplements could help to counteract the development of AD or slow down its progression, the researchers say.