What is already known on this topic
One of the main drivers of inflammatory bowel disease (IBD) is an excessive response of specific immune cells, called CD4+ T cells, to the gut microbiota. Previous studies have shown that overactive CD4+ T cells target flagellin proteins, the building blocks of swimming appendages used by many bacterial species to move around.What this research adds
Researchers have developed a method that eliminates overactive CD4+ T cells and stimulates the proliferation of regulatory immune cells that limit excessive immune responses. Injecting this treatment into mice with gut inflammation reduced the number of pathogenic CD4+ T cells and suppressed overactive immunity. The treatment also helped to eliminate pathogenic CD4+ T cells in blood samples from people with Crohn’s disease.Conclusion
The findings suggest that the combined approach to IBD treatment could be used in clinical trials. The same strategy could also help to treat other inflammatory or autoimmune diseases such as type 1 diabetes and multiple sclerosis, the researchers say.
Inflammatory bowel disease (IBD), which affects more than 0.3% of people in developed countries, is a term for debilitating disorders that involve long-term inflammation of the digestive tract. Now, researchers have developed a two-pronged treatment strategy — consisting of an engineered peptide and an FDA-approved drug — that could help to reduce gut inflammation.
The findings, published in Science Immunology, suggest that the combined approach to IBD treatment could be used in clinical trials.
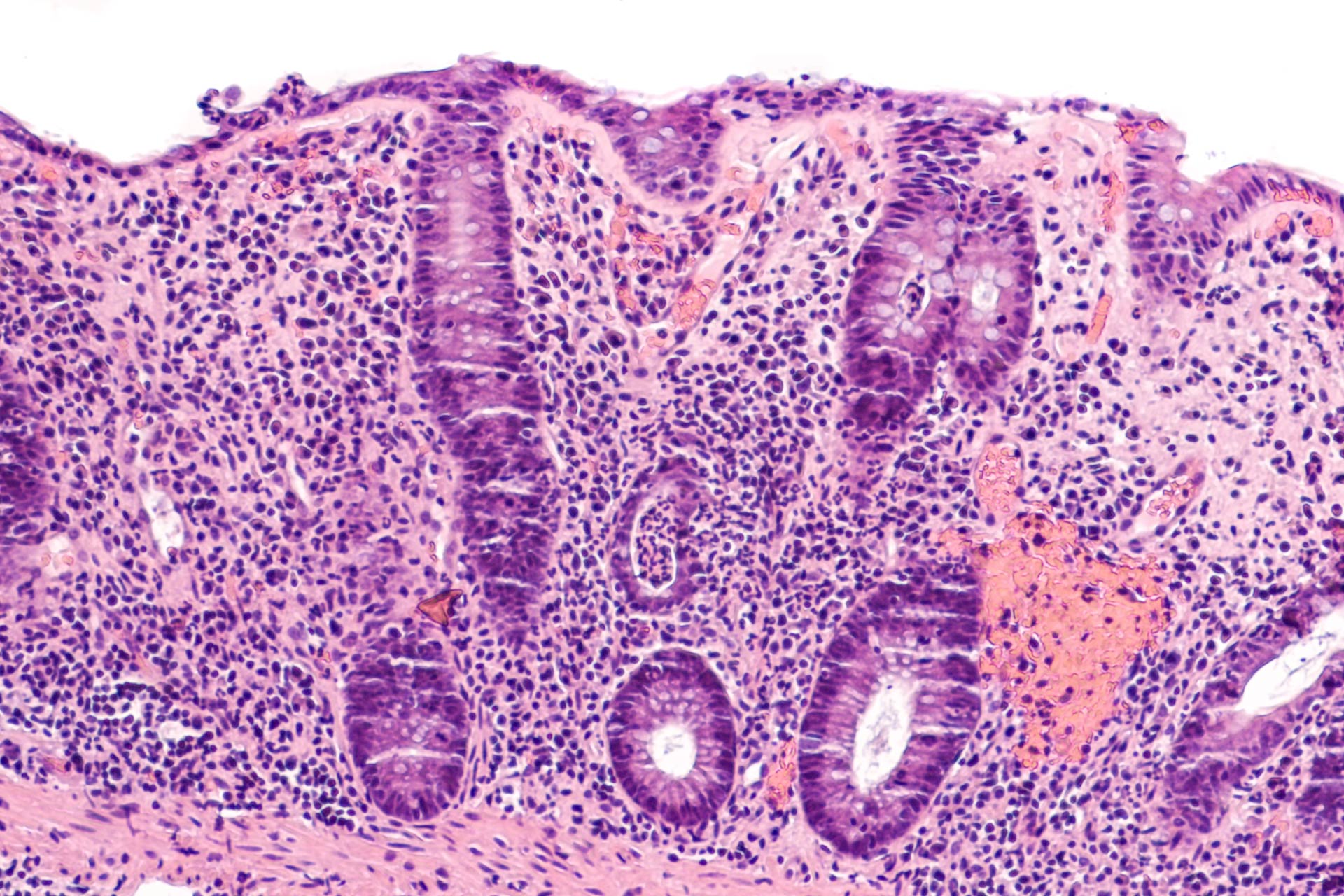
IBD include ulcerative colitis, which is characterized by inflammation of the lining of the gut, and Crohn’s disease, which often can involve the deeper layers of the digestive tract. Both disorders usually are characterized by diarrhea, fatigue, and weight loss.
One of the main drivers of IBD is an excessive response of specific immune cells, called CD4+ T cells, to the gut microbiota. Previous studies have shown that overactive CD4+ T cells target flagellin proteins, the building blocks of swimming appendages used by many bacterial species to move around.
Looking for a way to reduce gut inflammation in IBD, Charles Elson at the University of Alabama at Birmingham and his colleagues developed a method that eliminates overactive CD4+ T cells and stimulates the proliferation of regulatory immune cells that limit excessive immune responses.
Dampening immunity
To develop the potential treatment, the researchers first created an engineered peptide that includes parts of bacterial flagellin proteins. Then, they delivered the peptide to a mix of immune cells to isolate CD4+ T cells and activate them. Next, the team treated the activated cells with rapamycin, an FDA-approved drug that has immunosuppressive activity. Rapamycin was effective at eliminating CD4+ T cells grown in a lab dish, the researchers found.
Injecting the combination treatment into mice with gut inflammation reduced the number of pathogenic CD4+ T cells and suppressed overactive immunity. The treatment also helped to eliminate pathogenic CD4+ T cells in blood samples from people with Crohn’s disease.
“This study demonstrates an amelioration of immune-mediated inflammatory disease through peripheral ablation of [CD4+ T cells],” the researchers say. “This approach was shown effective in preventing colitis in a T cell transfer mouse model and had similar inhibitory effects on microbiota flagellin–specific CD4+ T cells isolated from [peripheral blood cells] of patients with Crohn’s disease, indicating a potential clinical application for this approach in IBD prevention and treatment.”
The same strategy could also help to treat other inflammatory or autoimmune diseases such as type 1 diabetes and multiple sclerosis, the researchers say.