What is already known
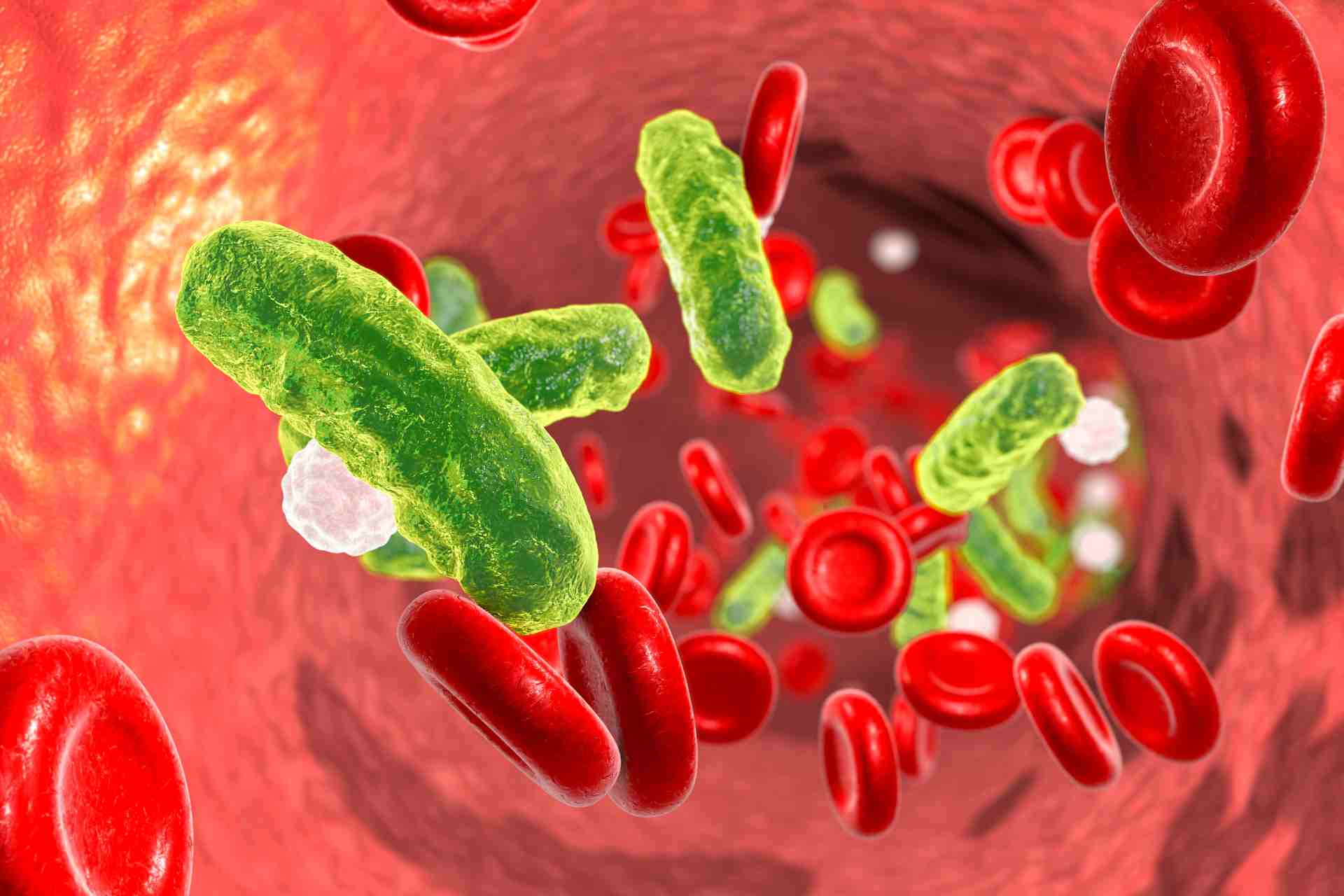
Bloodstream infection occurs when bacteria or fungi get into the blood. Some gut microbes may contribute to bloodstream infection by translocating from the gut to the blood of vulnerable people. But so far there’s little evidence linking these infections to the gut microbiota in critically ill patients.
What this research adds
Researchers analyzed the microbes present in 57 critically ill patients with bloodstream infection as well as the patients’ gut microbiotas. In about half of the cases, the team identified gut microbes that matched the species present in the blood infection. Among 23 bloodstream microorganisms analyzed, 14 were also present in the gut, and 6 were identical strains in the blood and gut.
Conclusions
The findings link the gut microbiota and the microorganisms responsible for bloodstream infection in critically ill patients. They also suggest that some microbes in bloodstream infection originate from the gut.
Bloodstream infections are a major cause of death in hospitalized patients, especially those who are critically ill or have a weakened immune system. New research suggests that some microbes in blood infection originate from the gut.
The findings, published in PLOS One, link the gut microbiota and the microorganisms responsible for these infections, which occur when bacteria or fungi get into the blood, in some hospitalized patients.
Some gut microbes may contribute to bloodstream infection by translocating from the gut to the blood of vulnerable people. But so far there’s little evidence linking these infections to the gut microbiota in critically ill patients.
To fill this knowledge gap, Christopher Gu at the University of Pennsylvania School of Medicine in Philadelphia and his colleagues analyzed the microbes present in 57 critically ill patients with bloodstream infection as well as the patients’ gut microbiotas.
Matching microbes
The researchers enrolled 139 adults admitted to the medical ICU of the Hospital of the University of Pennsylvania for whom stool samples were available. Of the study participants, 57 had blood infection.
Compared to healthy people, critically ill patients overall had lower gut microbiota diversity. The composition of the gut microbiota of some critically ill patients was similar to that of healthy individuals, while others had a microbiota dominated by a few bacterial groups, such as Proteobacteria or Firmicutes.
In about half of the cases, the researchers identified gut microbes that matched the species present in the blood infection. Among 23 bloodstream microorganisms analyzed, 14 were also present in the gut and 6 were identical strains in the blood and gut. These included Klebsiella pneumoniae, Escherichia coli, Proteus mirabilis, Pseudomonas aeruginosa and Enterococcus faecalis.
Identity confirmation
The team also identified one patient who had a bloodstream infection with Achromobacter insolitus, a bacterium that was recently isolated from various human clinical samples. Further analyses revealed that A. insolitus is present in the gut microbiota at low abundance.
However, because the patient had a respiratory tract infection with Achromobacter bacteria, the lungs may have been responsible for the bloodstream infection despite the high levels of Achromobacter in the gut. “This patient appeared to have two independent strains of Achromobacter present, emphasizing the importance of sequence-based identity confirmation,” the researchers say.
The finding that some gut microbes were identical to those found in bloodstream infection and thus could have originated from the gut warrants further investigation, they add. “In addition, an avenue for future research is whether there might be benefit to interventions that suppress highly dominant communities in some critically ill patients using targeted antimicrobial prophylaxis or microbiome transplantation, or other microbiome-targeted therapeutics.”