What is already known
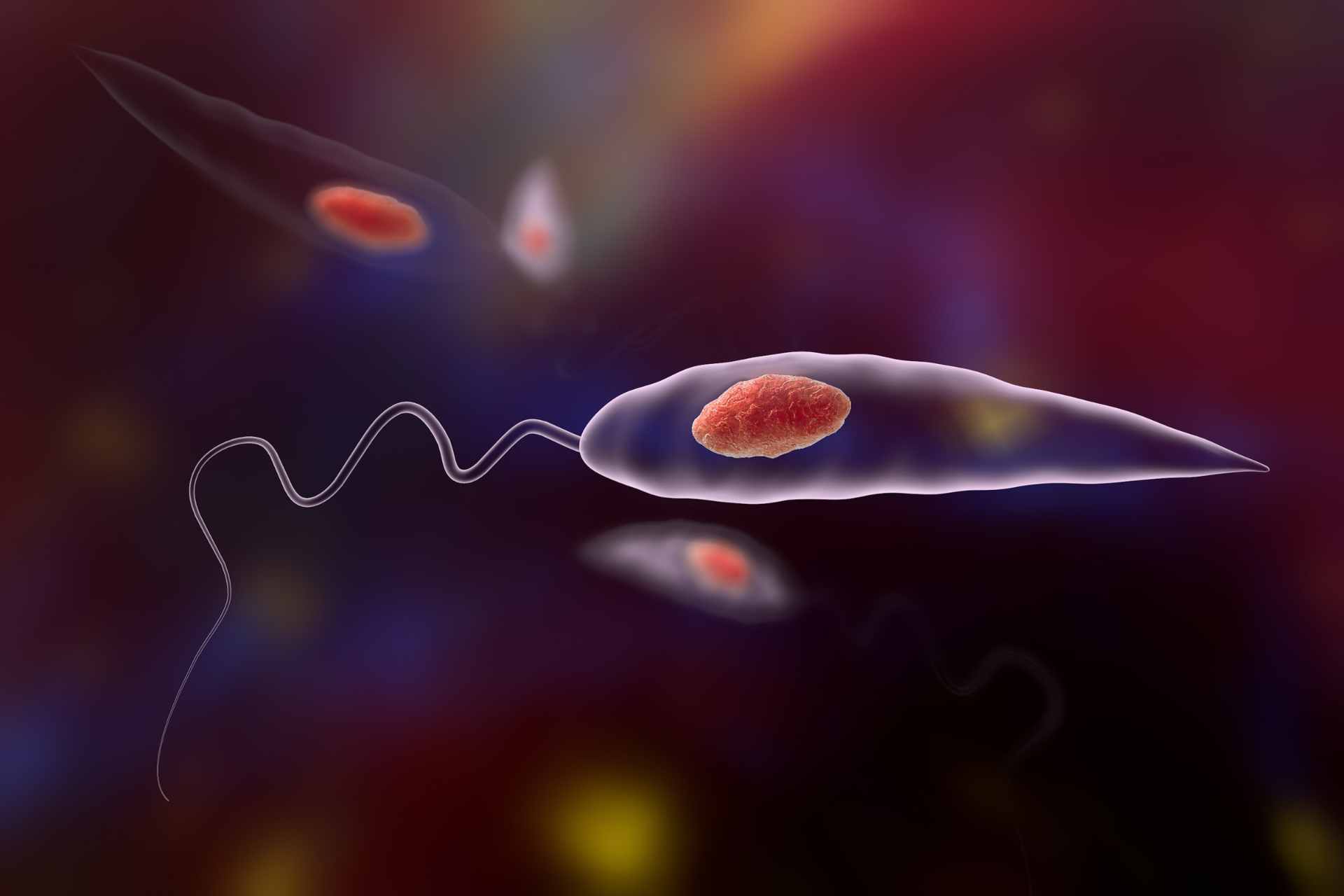
Leishmaniasis is a parasitic infection that can cause disfiguring skin lesions and for which there is no approved vaccine. People with cutaneous leishmaniasis develop chronic skin lesions and ulcers. But although previous studies in animal models suggest that the skin microbiota may play a role in cutaneous leishmaniasis, how skin bacteria influence the course of Leishmania infection remains unclear.
What this research adds
Working with mice and samples from 62 people with leishmaniasis, researchers have found that certain skin microbes, including Staphylococcus aureus, lead to slower healing of skin lesions. People with leishmaniasis also show heightened inflammatory responses, as suggested by an increased expression of inflammation-related genes in skin lesions. Dampening these responses reduces inflammation and accelerates skin healing in mice infected with Leishmania parasites.
Conclusions
The findings may inform new therapies to modulate the skin microbiota in people with leishmaniasis.
Leishmaniasis is a parasitic infection that can cause disfiguring skin lesions and for which there is no approved vaccine. New research suggests that the community of microbes living on the skin can influence the outcome of this disease.
The findings, published in Science Translational Medicine, may inform new therapies to modulate the skin microbiota in people with leishmaniasis. This, the researchers say, “might be accomplished by antibiotics, probiotics, and improved strategies for care of the leishmanial lesion.”
Leishmaniasis is caused by an infection with Leishmania parasites, which are spread by the bite of infected sand flies found in tropical and equatorial regions such as South America, the Middle East and Africa. People with cutaneous leishmaniasis develop chronic skin lesions and ulcers. But although previous studies in animal models suggest that the skin microbiota may play a role in cutaneous leishmaniasis, how skin bacteria influence the course of Leishmania infection remains unclear.
So, Camila Farias Amorim at the University of Pennsylvania in Philadelphia and her colleagues analyzed skin swabs from 62 people infected with Leishmania braziliensis, a species of the parasite mostly found in South America.
Bacterial burden
The researchers found that people who have high levels of bacteria in skin lesions tend not to respond to treatment. Bacteria that were enriched in lesions included Staphylococcus, Corynebacterium and Streptococcus.
High levels of Staphylococcus aureus in skin lesions were typically associated with treatment failure and delayed healing, suggesting that therapies that reduce S. aureus in leishmaniasis lesions can promote healing.
“People have been studying leishmaniasis for many years, and they’ve thought of it as being caused by one pathogen,” says study co-author Phillip Scott. “It’s not; it is a disease caused both by the parasite and the increased bacterial burden in lesions.”
Immune activation
People with leishmaniasis also showed increased inflammatory responses, the researchers found. Genes involved in inflammation, including those coding for the immune signaling molecule IL-1β, were expressed at higher levels in skin lesions.
Neutralizing IL-1β reduced inflammation and accelerated skin healing in mice infected with L. braziliensis, suggesting that this immune molecule can be a therapeutic target for cutaneous leishmaniasis in people.
“The important takeaway here is that the microbiome can modify the severity of the infections and influence the disease outcomes,” says study co-author Elizabeth Grice. “Our approach of studying human Leishmania infections to identify markers of disease severity, and then taking those findings into model systems to study mechanisms is very powerful.”