Asthma is a major cause of disability, poor quality of life world-wide and health resource utilization. The World Health Organisation (WHO) estimated that 262 million people suffered from asthma in 2019 and it caused 455 000 deaths. ResBiotic Nutrition Inc is a university startup out of the University of Alabama, Birmingham, USA, who partnered with Atlantia Clinical Trials Ltd., a world leading contract research organisation, to explore the effects of their novel supplement resB® Lung Support on lung function targeting the gut-lung axis. The gut-lung axis serves as a powerful means of communication between the gut microbiome and the inflammatory and immune microenvironment of the lungs. Patients with respiratory diseases often have gastrointestinal symptoms and show distinct gut microbiomes compared to healthy individuals¹. This new study asserts resB® Lung Support improves lung function through microbiome-mediated mechanisms along the gut-lung axis in asthmatic patients.
The gut-lung axis
Alterations in the gut microbial species and metabolites – also known as dysbiosis – have been linked to changes in immune response and inflammation in the lungs. Specific bacteria such as Lactobacillus species have been found to promote lung health by maintaining proper uptake of short chain fatty acids (SCFA) in both healthy and diseased populations². Metabolites from gut microbiota such as SCFA produced by gut bacteria travel through systemic circulation, thereby stimulating and promoting the differentiation of T-cells, which further supports anti-inflammatory and immunomodulatory actions in the lungs³.
Another downstream effect of dysbiosis, whether in the gut or the lungs, is inflammation associated with white blood cells called neutrophils. Neutrophilic inflammation is a common feature of many chronic lung diseases, and other cytokines including C-reactive protein (CRP) contributing to neutrophil recruitment and increased inflammatory response⁴. Dysbiosis in the gut can also be exacerbated with poor nutrient intake. Therefore, nutrition and a balanced gut microbiota are key components of a multi-factorial approach to support proper lung function⁵.
In a previously published trial of asthmatic patients, a Lactobacillus probiotic supplement taken once daily for eight weeks resulted in a significant improvement in lung function in terms of Forced Expiratory Volume in one second (FEV1%) and Forced Vital Capacity (FVC) measured by spirometry⁶. These tests calculate the amount of air that a person can force out of their lungs in 1 second (FEV1%) and the total amount of air exhaled during the FEV test (FVC). This study was significant as it was conducted with a robust design: a randomized, double-blinded, placebo-controlled trial. Another clinical study of probiotics, primarily conducted in children, have also shown improvements in asthma severity, allergic response, and immune biomarkers⁷.
About this study
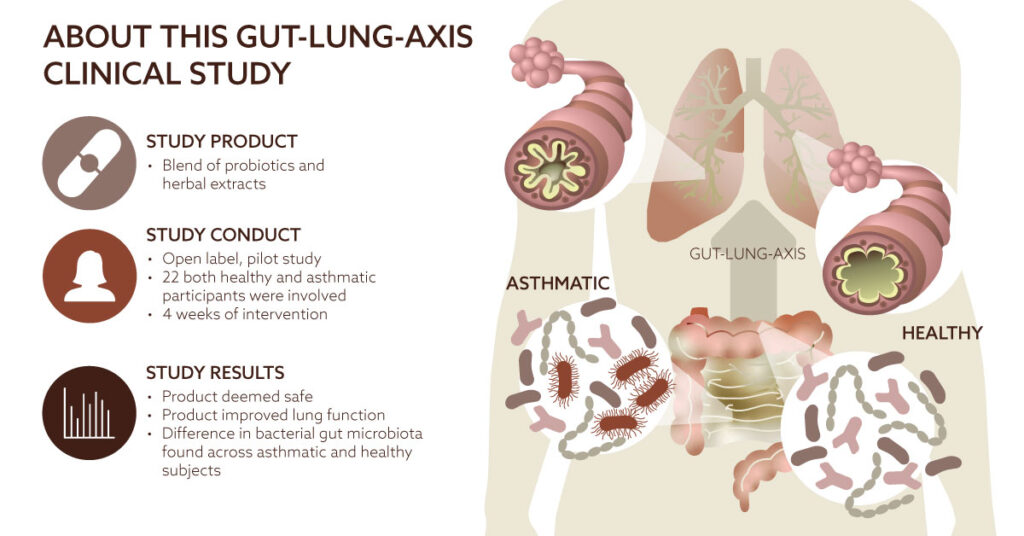
The research team was led by ResBiotic Nutrition Inc., Birmingham, USA. Their goal was to assess the safety of a probiotic in asthmatic and healthy participants and to explore its impact on lung function. They collaborated with Atlantia Clinical Trials who designed and carried the clinical outcomes of this study. The study was an open-label, pilot, cohort study to evaluate the safety of a 4-week intake of resB® Lung Support in asthma and healthy participants. The product was a blend of three probiotic Lactobacillus strains, namely L. plantarum, L. acidophilus, L. rhamnosus and three herbal extracts, turmeric, holy basil, and vasaka. The study focused on the vital signs and adverse events to assess the safety, whereas changes were documented for lung function measured by spirometry and questionnaires such as Saint George’s Respiratory Questionnaire (SGRQ) to measure respiratory health quality of life.
The results
resB® Lung Support was found to be safe and tolerable in asthmatic and healthy participants. The statistically significant improvements in lung function (FEV1%, and positive trends in FVC) and SRGQ are promising. This improvement may have been due to the significant uptick in serum SCFA which traveled through systemic circulation to reach the lung microenvironment. resB® Lung Support is thought to improve lung function by supplementing microbes in the gut to increase SCFA production in systemic circulation in patients with asthma.
Looking ahead
In the future, microbiome amplicon sequencing and analysis of gut and lung microbiota in patients with respiratory conditions may provide an insight into the possible microbial changes associated with resB® Lung Support. The respiratory microbiome has been shown to play roles in human health and disease and is an area of rapidly emerging interest in pulmonary medicine. It is necessary to understand the relationship between microbiome changes and the development of lung disease to identify new pathway targets, which will bring major breakthroughs in targeted screening models and microbial-based therapies with the ultimate goal of improving patient care and outcomes⁸.
In conclusion, the study presented positive results as the safety and tolerability of resB® Lung Support was confirmed. The improvements in lung function associated with the Lactobacillus probiotic and herbal blend were accompanied by potentially beneficial increases in SCFA in asthmatic patients. Clinical relevance of these findings affects people with and without existing respiratory conditions who are seeking a means to support their lung health.
Content sponsored by Atlantia Clinical Trials
References
- Bowerman KL, Rehman SF, Vaughan A, Lachner N, Budden KF, Kim RY, et al. Disease associated gut microbiome and metabolome changes in patients with chronic obstructive pulmonary disease. Nat Commun. 2020;11(1):5886.
- Kumar A, Alrefai WA, Borthakur A, Dudeja PK. Lactobacillus acidophilus counteracts enteropathogenic E. coli-induced inhibition of butyrate uptake in intestinal epithelial cells. Am J Physiol Gastrointest Liver Physiol. 2015;309(7):G602-7.
- Arpaia N, Campbell C, Fan X, Dikiy S, van der Veeken J, deRoos P, et al. Metabolites produced by commensal bacteria promote peripheral regulatory T-cell generation. Nature. 2013;504(7480):451-5
- Vaguliene, N.; Zemaitis, M.; Lavinskiene, S.; Miliauskas, S.; Sakalauskas, R. Local and systemic neutrophilic inflammation in patients with lung cancer and chronic obstructive pulmonary disease. BMC Immunol. 2013, 14, 36.
- Shin, N.-R.; Whon, T.W.; Bae, J.-W. Proteobacteria: Microbial signature of dysbiosis in gut microbiota. Trends Biotechnol. 2015, 33, 496–503.
- Sadrifar S, Abbasi-Dokht T, Forouzandeh S, Malek F, Yousefi B, Salek Farrokhi A, et al. Immunomodulatory effects of probiotic supplementation in patients with asthma: a randomized, double-blind, placebo-controlled trial. Allergy, Asthma & Clinical Immunology. 2023;19(1):1.
- Huang CF, Chie WC, Wang IJ. Efficacy of Lactobacillus Administration in School-Age Children with Asthma: A Randomized, Placebo-Controlled Trial. Nutrients. 2018;10(11).
- Ma PJ, Wang MM, Wang Y. Gut microbiota: A new insight into lung diseases. Biomed Pharmacother. 2022 Nov;155:113810.