[toc]
What is already known on this topic
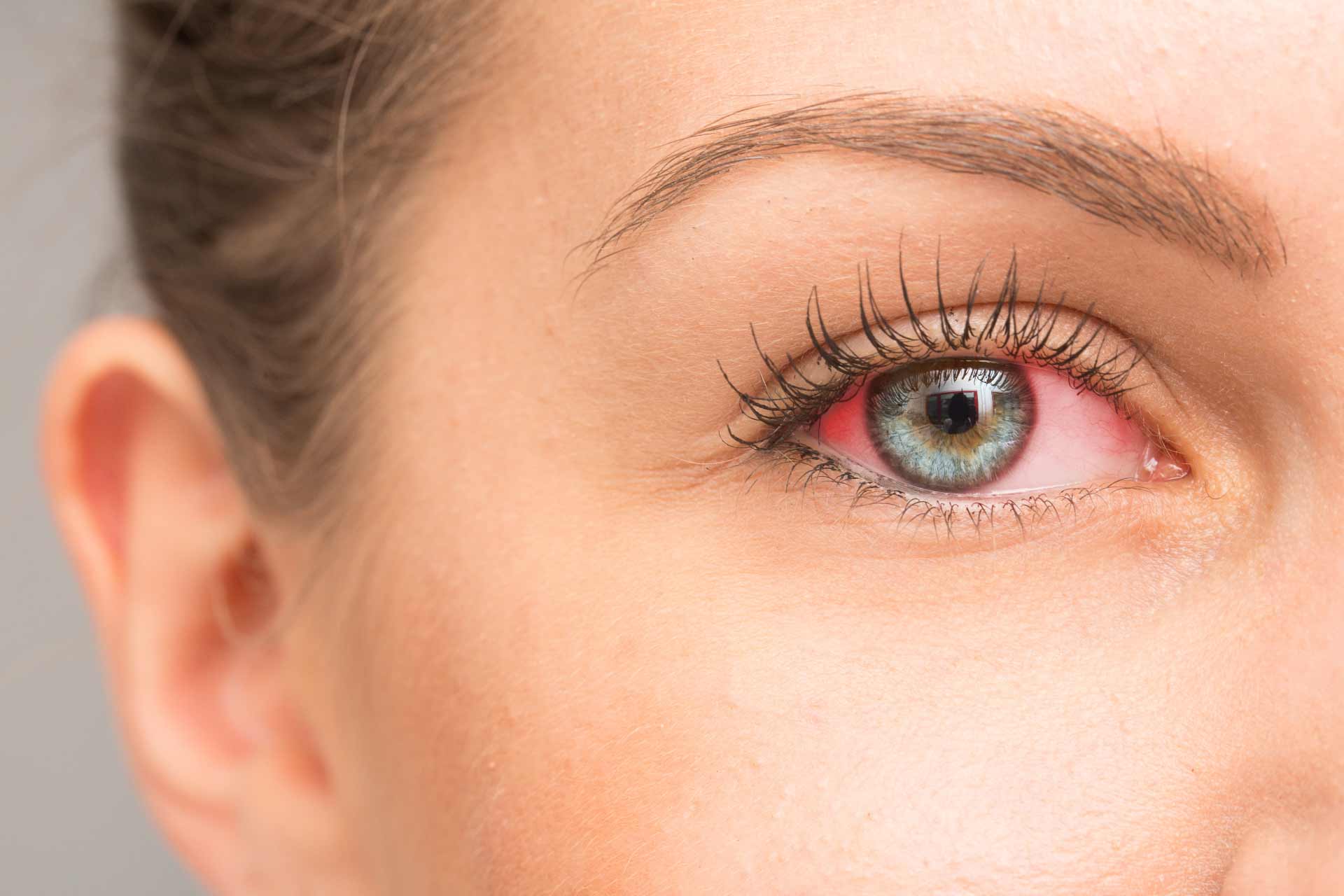
Uveitis is a form of eye inflammation that causes eye redness, pain and blurred vision, and it can even lead to blindness. In many cases, the specific cause of uveitis isn’t clear, and the disorder is considered an autoimmune disease. Recent studies have showed that an altered gut microbiota may modulate immune responses in people with uveitis.
What this research adds
Researchers have found decreased levels of secondary bile acids, which result from gut bacteria’s metabolism, in the stool and blood of mice with autoimmune uveitis. Restoring the levels of microbiota-derived bile acid deoxycholic acid (DCA) reduces the severity of uveitis, likely by inhibiting the production of pro-inflammatory molecules in immune cells called dendritic cells. DCA appears to inhibit the production of inflammatory molecules by dendritic cells through the activation of the bile acid receptor TGR5. Compounds that activate TGR5 also inhibit dendritic cells.
Conclusions
The findings indicate that bile acids metabolism plays an important role in immune responses. The work also suggests that microbiota-derived bile acids can be a therapeutic target in autoimmune uveitis.
Uveitis is a form of eye inflammation that causes eye redness, pain and blurred vision, and it can even lead to blindness. In many cases, the specific cause of uveitis isn’t clear, and the disorder is considered an autoimmune disease. Now, researchers have found that the levels of microbiota-derived bile acids can influence the severity of uveitis — at least in mice.
The findings, published in Cell Reports, indicate that bile acids metabolism plays an important role in immune responses. The work also suggests that microbiota-derived bile acids can be a therapeutic target in autoimmune uveitis.
Uveitis is usually treated with anti-inflammatory and immunosuppressive drugs. “But despite this therapy, many eyes still go blind,” the researchers say. “Therefore, there is an ongoing search to elucidate the mechanisms involved in the pathogenesis of uveitis, which might lead to the discovery of potential therapeutic targets,” they add.
Recent studies have showed that an altered gut microbiota may modulate immune responses in people with uveitis. For example, transferring feces from people with uveitis to mice worsens eye inflammation in the animals. Researchers have also observed an altered microbiota composition in individuals with uveitis and other autoimmune or inflammatory diseases.
To further investigate the link between uveitis and gut microbes, a team led by Hong Li at Chongqing Branch of National Clinical Research Center for Ocular Diseases tested bile acids and microbiota composition in a mouse model of autoimmune uveitis.
Bile acid balance
Produced in the liver and metabolized by gut bacteria, bile acids are involved in the control of the immune system and have been implicated in conditions such as inflammatory bowel disease and type 1 diabetes.
First, Li and colleagues analyzed the gut microbiota of mice with autoimmune uveitis and healthy mice. Ruminococcaceae, Lachnospiraceae, and Eggerthellaceae were abundant in control mice, whereas Prevotellaceae were predominant in mice with uveitis, the researchers found.
Previous work has suggested that, in the presence of bile acids, Ruminococcaceae and Lachnospiraceae convert primary bile acids into secondary bile acids. To investigate whether the composition of bile acids could contribute to the development of autoimmune uveitis, the researchers looked at the levels of bile acids in the mice’s stool and blood. Those with autoimmune uveitis had lower levels of secondary bile acids compared to healthy mice, the team found.
Immune interaction
Restoring the levels of microbiota-derived bile acids reduced the severity of uveitis, the researchers found. The team discovered that feeding mice with a diet rich in the secondary bile acid deoxycholic acid (DCA) improved symptoms of uveitis. DCA acts by regulating the function of immune cells called dendritic cells and reducing the production of specific inflammatory immune molecules.
Further experiments indicated that DCA inhibits the production of inflammatory molecules through the activation of the bile acid receptor TGR5. Both DCA and TGR5 blocked the activation of human-derived dendritic cells, and so did compounds that activate TGR5, the researchers found.
“We show that gut microbiota-derived secondary bile acids might be key regulators in the pathogenesis of autoimmune uveitis,” the authors say. “Gut microbiota and secondary bile acid composition as well as TGR5 signaling may provide potential therapeutic targets for the treatment of autoimmune and inflammatory diseases, including uveitis.”