What is already known
Some gut bacteria can migrate across the gut barrier and drive the development of chronic inflammatory conditions. However, it’s unclear how potentially harmful bacteria can live in the gut of people with no apparent health consequences.
What this research adds
Researchers introduced Enterococcus gallinarum, a potentially harmful bacterial species, in the gut of germ-free mice. Over time, the bacteria diverged into two distinct populations: one that behaved like the ancestral strain and another that gained the ability to escape the intestine and persist in the liver. This population was able to temporarily evade detection and clearance by the mice’s immune system and trigger inflammatory symptoms. The researchers observed similar patterns of divergent evolution and increased immune evasion in strains of Lactobacillus reuteri that were introduced into germ-free mice.
Conclusions
The findings may in part explain why the risk of developing microbiota-driven diseases increases with age, and why some people with potentially harmful bacteria never get sick.
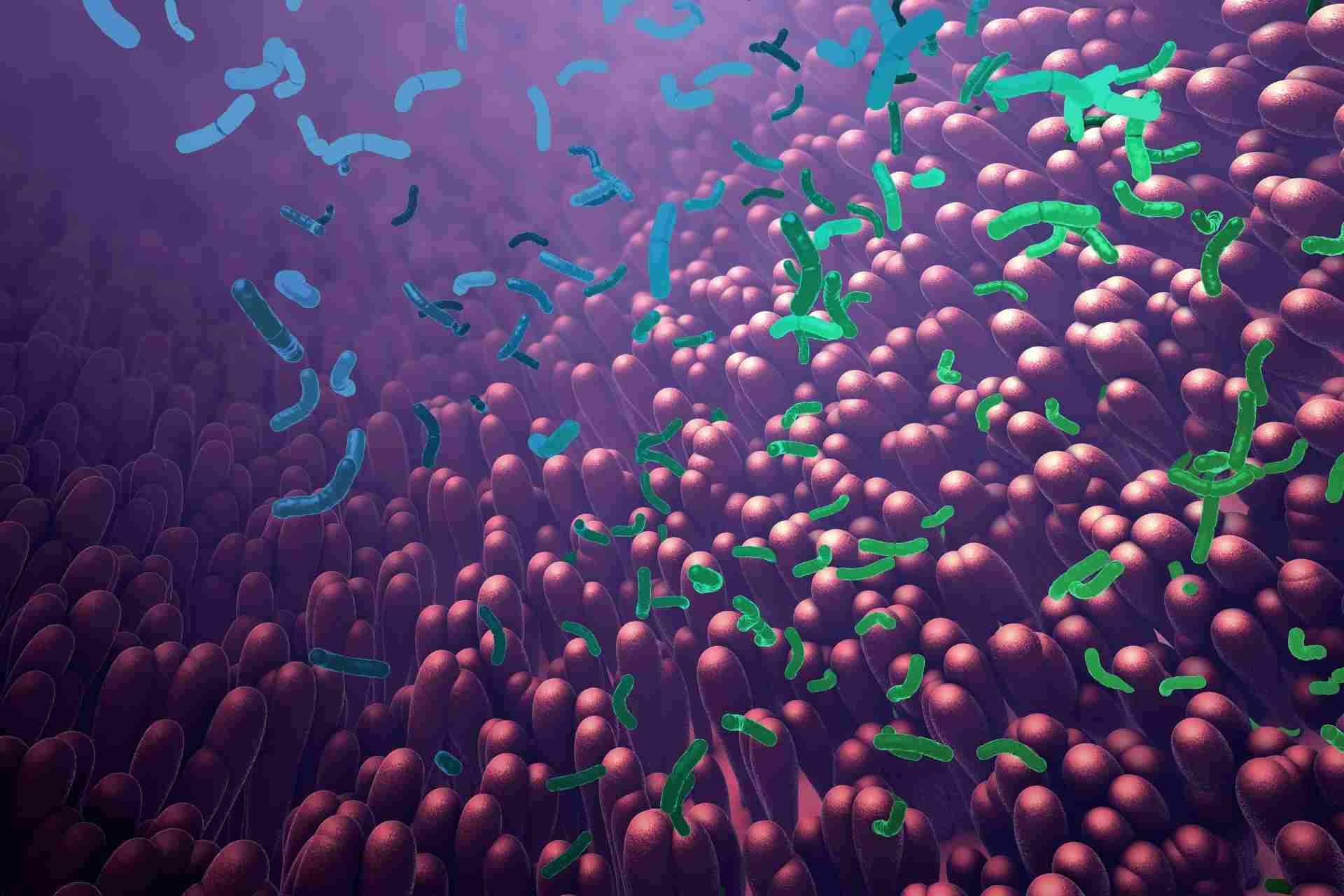
Some gut bacteria can migrate across the gut barrier and drive the development of chronic inflammatory conditions, but it’s unclear how potentially harmful bacteria can live in the gut of people with no apparent health consequences. New findings in mice may explain why.
The work, published in Nature, shows that gut bacteria can become harmful over time by gaining the ability to escape the intestine and persist in other organs where they can trigger chronic inflammation.
Understanding how gut bacteria evolve within their host could help to develop new therapeutic interventions that may reduce the risk of microbiota-driven diseases.
“Gut commensals with pathogenic potential, referred to as pathobionts, are believed to have causal roles in a diverse array of inflammation-associated diseases, ranging from inflammatory bowel disease to metabolic syndrome,” the researchers say.
However, they add, “pathobionts are also detected in ostensibly healthy humans,” but the factors that influence microbiota-driven inflammatory disease are unclear. The researchers hypothesized that ‘within-host evolution’, a phenomenon through which gut bacteria adapt and evolve, may make these microbes more harmful over time.
To test this hypothesis, the team — led by Noah Palm at Yale University School of Medicine — introduced the model pathobiont Enterococcus gallinarum in mice grown in the absence of bacteria.
Bacterial translocation
E. gallinarum is found in more than 6% of human gut microbiotas and its translocation to lymph nodes and liver accelerates the development of autoimmune disorders in mice. E. gallinarum has also been found in liver biopsies from people with autoimmune diseases.
The researchers found that over time, E. gallinarum diverged into two distinct populations: one that behaved like the ancestral strain and another that gained the ability to escape the intestine and persist in the liver.
Mutations in the genes walK and manX were detected in the population that behaved like the ancestral strain, whereas mutations in manY, lacE, ypdA and immR were more common in the population that translocated to the liver. Some of these genes regulate broad transcriptional programs that may influence multiple features of bacterial behavior.
Immune evasion
Compared to the ancestral strain, the population that translocated to the mice’s liver was able to temporarily evade detection and clearance by the mice’s immune system, the researchers found. These bacteria were more resistant to killing by antimicrobial peptides produced by the host and were able to escape a form of clearance, called phagocytosis, by specific immune cells.
Further experiments revealed that the population that translocated to the liver triggered inflammation and exacerbated symptoms of autoimmune conditions.
The researchers observed similar patterns of divergent evolution and increased immune evasion in strains of Lactobacillus reuteri that were introduced into germ-free mice. However, Bacillus fragilis did not translocate to the liver of mice, the team found.
“Our results demonstrate that within-host evolution of a gut pathobiont can facilitate bacterial translocation and therefore reveal a previously undescribed microbial source of stochasticity in the development and progression of diverse microbiota-driven pathologies,” the researchers say.