• Bacterial shifts
• Lactose-free diet
What is already known on this topic
Alterations of the gut microbiota composition have been linked to many health conditions, including the clinical outcome of bone marrow transplant. But the factors that trigger these changes are still unclear.What this research adds
Researchers found that changes in the proportion of several bacterial species, in particular an increase in Enterococcus faecium, trigger inflammation and immune-mediated damage in response to bone marrow transplant. This increase in E. faecium is associated with graft-versus-host disease, a fatal immune condition that occurs after transplant procedures, when immune cells from the donor attack the recipient patient’s tissues. In mice, a lactose-free diet reduced the growth of E. faecium and its negative effects, suggesting that the increase in enterococci depends on dietary lactose.Conclusion
The findings suggest that gut microbes such as E. faecium are able to stimulate the immune system and trigger inflammation.
Changes in the proportion of some gut bacteria could promote graft-versus-host disease, a fatal immune condition that occurs after transplant procedures, when immune cells from the donor attack the recipient patient’s tissues. That’s according to a new study, which also showed how a lactose-free diet reduced the severity of graft-versus-host disease in mice.
The findings, published in Science, could help inspire new non-antibiotic-based therapeutic strategies for reducing inflammatory disease after transplant procedures and improving clinical outcomes.
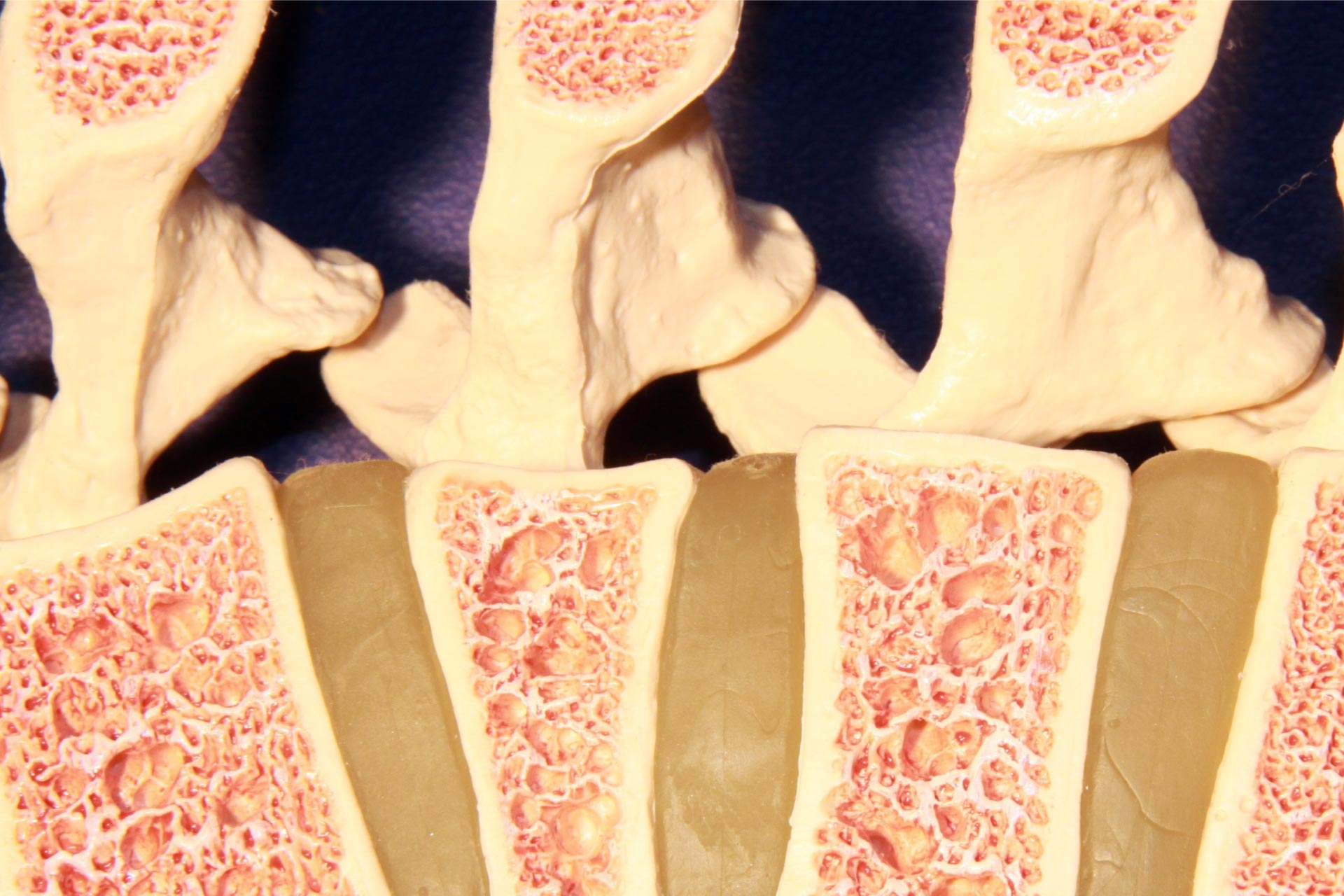
Previous work suggested that the gut microbiota influences the clinical outcome of bone marrow transplant. To investigate this further, Christoph Stein-Thoeringer at the Memorial Sloan Kettering Cancer Center and his colleagues analyzed the fecal microbiota of 1325 people who received a bone marrow transplant, which is used to treat blood cancers such as leukemias and lymphomas.
Bacterial shifts
In the guts of bone marrow recipients, the researchers observed an increase in the proportion of enterococci occurring shortly after receiving transplants. The rise in enterococci was associated with increased rates of lethal graft-versus-host disease. Analyses of the bacterial genomes from transplant recipients showed increased expression of enzymes involved in degradation of the sugars lactose and galactose.
The team found a rise in enterococci, as well as a reduction of commensal Clostridia, also in several mouse models of bone marrow transplant. The reduction of Clostridia led to decreased levels of butyrate, a microbial metabolite that has anti-inflammatory effects. The expansion of enterococci, in particular Enterococcus faecium, was instead accompanied by increased levels of these bacteria in the lymph nodes, which suggested that the microbes had translocated beyond the gut barrier.
Mice undergoing bone marrow transplant also had reduced levels of lactase, the enzyme that degrades lactose, in their gut. This reduction appeared to be mediated by T cell-dependent inflammation.
Lactose-free diet
Feeding mice a lactose-free diet reduced the growth of E. faecium and the signs of immune cells activation, as well as the severity of graft-versus-host disease. Also, lactose-intolerant patients had a greater overall abundance of enterococci.
The results suggest that the increase in enterococci in the gut of transplant patients depends on dietary lactose, but it’s unclear whether lactose intake influences the severity of graft-versus-host disease.
Because bacterial species such as E. faecium are able to stimulate the immune system and trigger inflammation, the diet of bone marrow transplant patients should be adapted to avoid potentially fatal shifts in their gut microbiota, the researchers say.