What is already known
Several studies have shown that gut microbes can produce toxins that damage DNA, induce tumor-promoting inflammation and reduce a person’s response to cancer treatment. For example, Fusobacterium nucleatum — an oral commensal that can cause different infections in the mouth — has been associated with the development of colorectal cancer.
What this research adds
In a Forum, Robert Holt discusses recent efforts to develop vaccines designed to boost a person’s immune response against cancer-promoting microbes such as F. nucleatum.
Conclusions
Vaccines against F. nucleatum and other onco-microbes may help prevent diseases such as colorectal cancer.
Several studies have shown that gut microbes can produce toxins that damage DNA, induce cancer-promoting inflammation and reduce a person’s response to cancer treatment. So, researchers are racing to develop targeted approaches against onco-microbes, as vaccines against tumor-promoting microorganisms may help prevent diseases such as colorectal cancer.
Writing in Cell Host & Microbe, Robert Holt, co-director of the cancer immunotherapy program at the University of British Columbia, discusses recent efforts to develop vaccines designed to boost a person’s immune response against some of these microorganisms.
The first microbes to be linked with cancer were Helicobacter pylori and human papillomavirus, but over the past decade it has become clear that several other microorganisms — including some commensal bacteria — could provoke tumor formation.
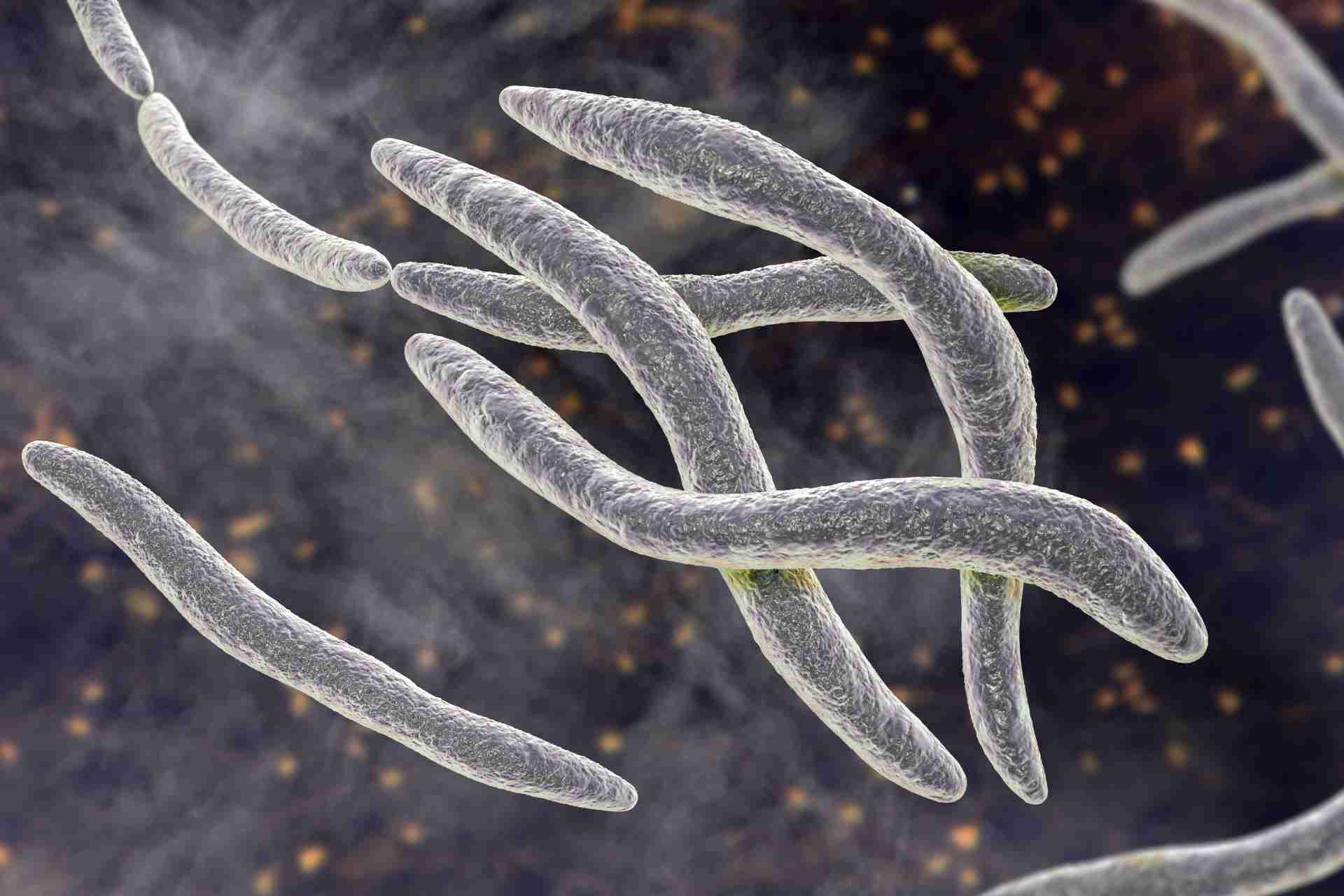
For example, individuals at high risk of developing colon cancer carry in their guts strains of Escherichia coli that produce a DNA-damaging toxin as well as strains of Bacteroides fragilis that induce severe diarrhea and colon inflammation and are able to cause cancer in mouse models. Fusobacterium nucleatum — an oral commensal that can cause different infections in the mouth — has also been associated with the development of colorectal cancer.
When a single microbe causes cancer, vaccines can be an effective cancer prevention strategy. In clinical trials, the first FDA-approved vaccine against human papillomavirus — the main cause of cervical cancer — was nearly 100% effective in preventing lesions that could lead to cancer. However, developing vaccine interventions for most bacterial pathogens isn’t straightforward.
“F. nucleatum, as an agent of tumor promotion and treatment resistance, presents some unique and unconventional opportunities for vaccine intervention,” Holt says.
Tumor-promoting antigens
F. nucleatum colonizes a baby’s mouth in the first months of life, and, by the age of one, it becomes one of the main oral commensals. Because F. nucleatum is so abundant in the mouth, “we are all prone to systemic exposure by everyday activities that elicit transient bacteremia, including tooth brushing, and even just chewing, which is an unsettling thought,” Holt says.
In people with a normal immune system, these exposures are harmless, but they can become problematic in people with weakened immunity. “Here, a vaccine that elicits antibodies that block specific mechanisms of F. nucleatum tumor homing and tumor promotion could be beneficial,” Holt says.
A vaccine could be targeted towards tumor-promoting antigens such as Fap2 and RadD, two F. nucleatum outer-membrane proteins that bind carbohydrates on the surface of tumor cells. Both Fap2 and RadD can suppress the immune system. Another F. nucleatum surface protein, FadA, has been shown to bind to tumor cells and activate a specific signaling pathway that stimulates cell proliferation.
“Since Fap2 and FadA directly mediate microbe-tumor interaction, an antibody response against them may be effective in blocking tumor colonization and mitigating immune inhibition,” Holt says.
Combined interventions
People with tumors containing F. nucleatum who have relapsed with treatment-resistant disease may benefit the most from F. nucleatum vaccines. In this case, Holt notes that it may be useful to add antibiotic treatments to vaccine interventions against the bacterium.
“For example, better outcomes might be possible if, after standard therapy, an aggressive short-term course of antibiotics is used to clear F. nucleatum from sites of minimal residual disease and metastatic lesions, and then an effective vaccine is deployed to consolidate remissions by preventing re-infection and recurrence of treatment-refractory tumors,” he says.
A potential concern is that, since F. nucleatum is an important oral commensal, its absence could lead to dysbiosis and increase the risk of mouth infections. Another concern is related to the cross-reactive immunity to beneficial microbes that a vaccine against F. nucleatum may elicit.
“These risks must be weighed against the potential benefits of an effective F. nucleatum vaccine for cancer control,” Holt says. But, he adds, there is no reason to wait. “The journey from pathogen identification and characterization to vaccine design, testing, optimization, and roll-out is known to be long and onerous, so we shouldn’t delay.”