Researchers have discovered how specific gut bacteria help the immune system to attack tumors. The study, done in mice, shows that some gut microbes produce a metabolite that boosts the effect of a class of cancer drugs. The effects are reproducible across several types of cancer, including colorectal cancer, bladder cancer, and skin cancer.
The findings, published in Science, could help to explain why immunotherapy, a type of cancer therapy that unleashes a person’s immune system against tumor cells, works in some cases but not in others.
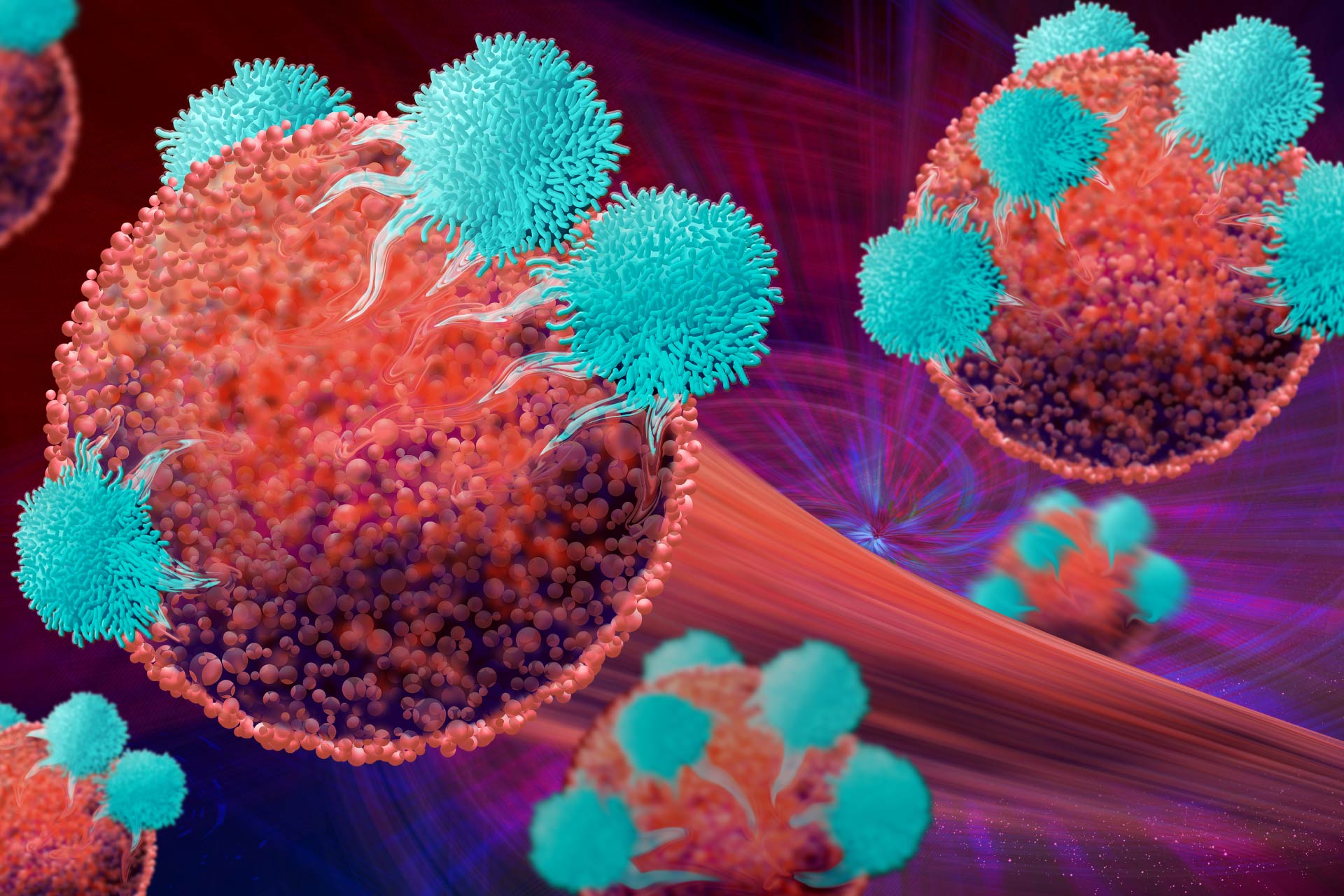
“Recent studies have provided strong evidence that gut microbiota can positively affect anti-tumor immunity and improve the effectiveness of immunotherapy in treating certain cancers—yet, how the bacteria were able to do this remained elusive,” says study lead author Kathy McCoy at the University of Calgary. “We’ve been able to build on that work by showing how certain bacteria enhance the ability of T cells, the body’s immunity soldiers that attack and destroy cancerous cells.”
To find out which microbes can boost the activity of immunotherapy drugs, the researchers grew tumors from mice treated with immunotherapy and from mice that received no treatment.
Tumor bacteria
From the lab-grown tumors, the team was able to identify 21 bacterial species, seven of which were present only in immunotherapy-treated tumors.
Next, the researchers introduced the bacterial species present only in immunotherapy-treated tumors into mouse models for several types of cancer, including colorectal cancer, bladder cancer, and skin cancer. Three bacterial species—Bifidobacterium pseudolongum, Lactobacillus johnsonii, and Olsenella—boosted the efficacy of immunotherapy drugs.
The team found that B. pseudolongum modulated the mice’s response to immunotherapy by producing a metabolite called inosine, which is known to modulate immune responses. Akkermansia muciniphila, a microbe that is known to enhance the efficacy of some immunotherapy treatments in lung and kidney cancers, was also found in immunotherapy-treated tumors and was able to produce inosine.
Attacking tumors
In mice with colorectal cancer, the combination of inosine and immunotherapy activated the anticancer response of T cells, leading to a reduction in size of the tumors. Similar results were obtained in mice with skin cancer and bladder cancer. “Inosine interacts directly with T cells and together with immunotherapy, it improves the effectiveness of that treatment, in some cases destroying all the colorectal cancer cells,” says study first author Lukas Mager.
Although it’s still unknown whether the findings apply to people, the beneficial bacteria associated with improved response to immunotherapy in mice have also been found in human cancer. This suggests that inosine could be exploited to develop microbial-based adjuvant treatments for immunotherapy, the researchers say.
“Identifying how microbes improve immunotherapy is crucial to designing therapies with anti-cancer properties,” says McCoy. “We are in the early stage of fully understanding how we can use this new knowledge to improve efficacy and safety of anti-cancer therapy and improve cancer patient survival and well-being,” she says.