• Skin barrier
• Potential treatment
What is already known on this topic
The EGFR receptor is an important target for many cancer drugs, but these drugs can also cause severe skin rashes, which may decrease patients’ adherence to treatment.What this research adds
In mice, disrupting EGFR caused increased susceptibility to skin inflammation by hindering the function of skin stem cells, which normally help the skin barrier to heal after hair eruption. As a result, commensal bacteria such as Staphylococcus aureus could invade the skin through the broken skin barrier and lead to inflammation.Conclusion
The results show how the microbiota contributes to skin damage after treatment with EGFR inhibitors and reveal why these drugs cause severe skin side effects.
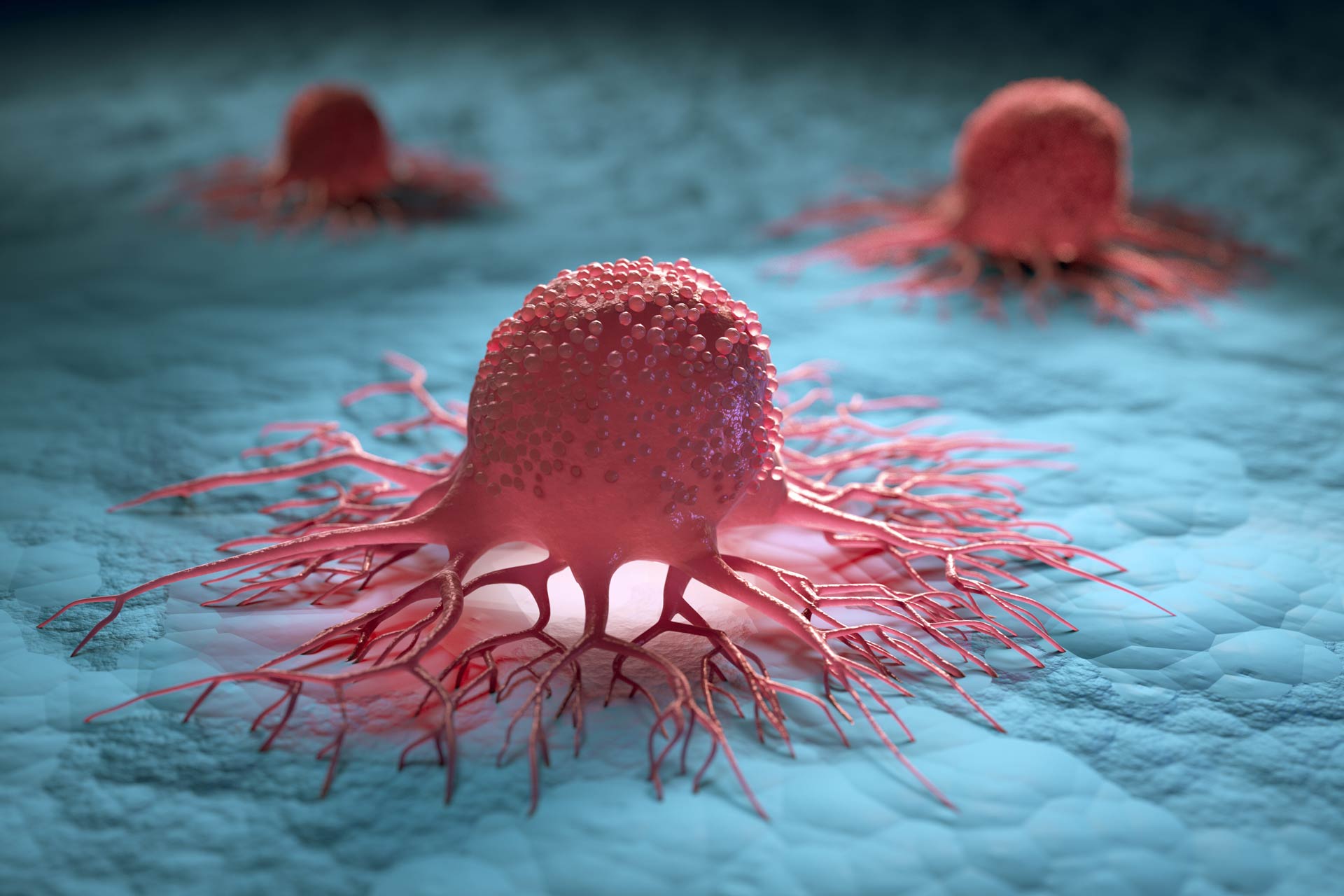
A common cancer treatment can allow commensal bacteria to invade growing hairs and cause skin irritation, according to a new study in mice. The findings, published in Science Translational Medicine, reveal why EGFR inhibitors, which are approved to treat cancers such as lung and colorectal cancer, cause severe skin side effects.
The EGFR receptor is an important target for many cancer drugs, but inhibiting this receptor does not only help to fight off cancer cells, it also causes severe skin rashes followed by Staphylococcus aureus infections, hitching, and hair alterations. These side effects may decrease patients’ adherence to treatment, and although antibiotics, corticosteroids, and moisturizers can alleviate some of the symptoms, no treatment can prevent skin damage.
To find out the causes of EGFR inhibitors’ damaging effects and identify potential treatments, a team of researchers led by Jörg Klufa and Thomas Bauer at the Medical University of Vienna studied mice that lack EGFR receptor in their skin.
Skin barrier
Mice lacking EGFR receptor in their skin showed skin barrier defects that were associated with inflammation at the hair follicles. Skin irritation was accompanied by the expression of pro-inflammatory molecules. This suggested that disrupting EGFR caused increased susceptibility to skin inflammation by hindering the function of skin stem cells, which normally help the skin barrier to heal after hair eruption.
As a result, commensal bacteria such as Staphylococcus aureus could invade the skin through the broken skin barrier and colonize the follicular opening of the erupting hair. There, the microbes triggered an additional immune response that led to chronic inflammation of the hair follicle.
Treating mice with antibiotics, which eliminated bacteria from the skin, reduced inflammation. But the mice’s skin barrier remained open and continued to express pro-inflammatory molecules.
Potential treatment
The researchers found that treating mice lacking EGFR with a growth factor called FGF7 preserved the skin barrier. This suggests that FGF7 could be used as a therapeutic approach to mitigate the side effects of disrupting EGFR.
But whether this strategy could treat skin damage in cancer patients receiving EGFR inhibitors is still unknown. The researchers note that more research is needed to work out the causes of the side effects of these cancer drugs and identify effective treatment options.