What is already known
Despite improved hygiene measures, infections that occur in the wound following an invasive surgical procedure remain a leading cause of post-surgery complications. But where surgical site infections come from and why they’re so resistant to antibiotics is unclear.
What this research adds
Researchers analyzed samples of bacteria from the noses, skin, and stool of more than 200 patients before they underwent spine surgery. Then, the team followed the patients for 90 days to compare the initial samples with any infections that occurred following surgery. About 86% of post-surgery infections originated from bacteria that were already present in the patients before the spine surgery, and nearly 60% of these infections were also resistant to the antibiotics used during the surgical procedure, the antiseptic used to clean the skin before incision, or both.
Conclusions
The findings may help clinicians to select more targeted antimicrobials based on where on the body the surgery is taking place or which type of bacteria inhabit that body site.
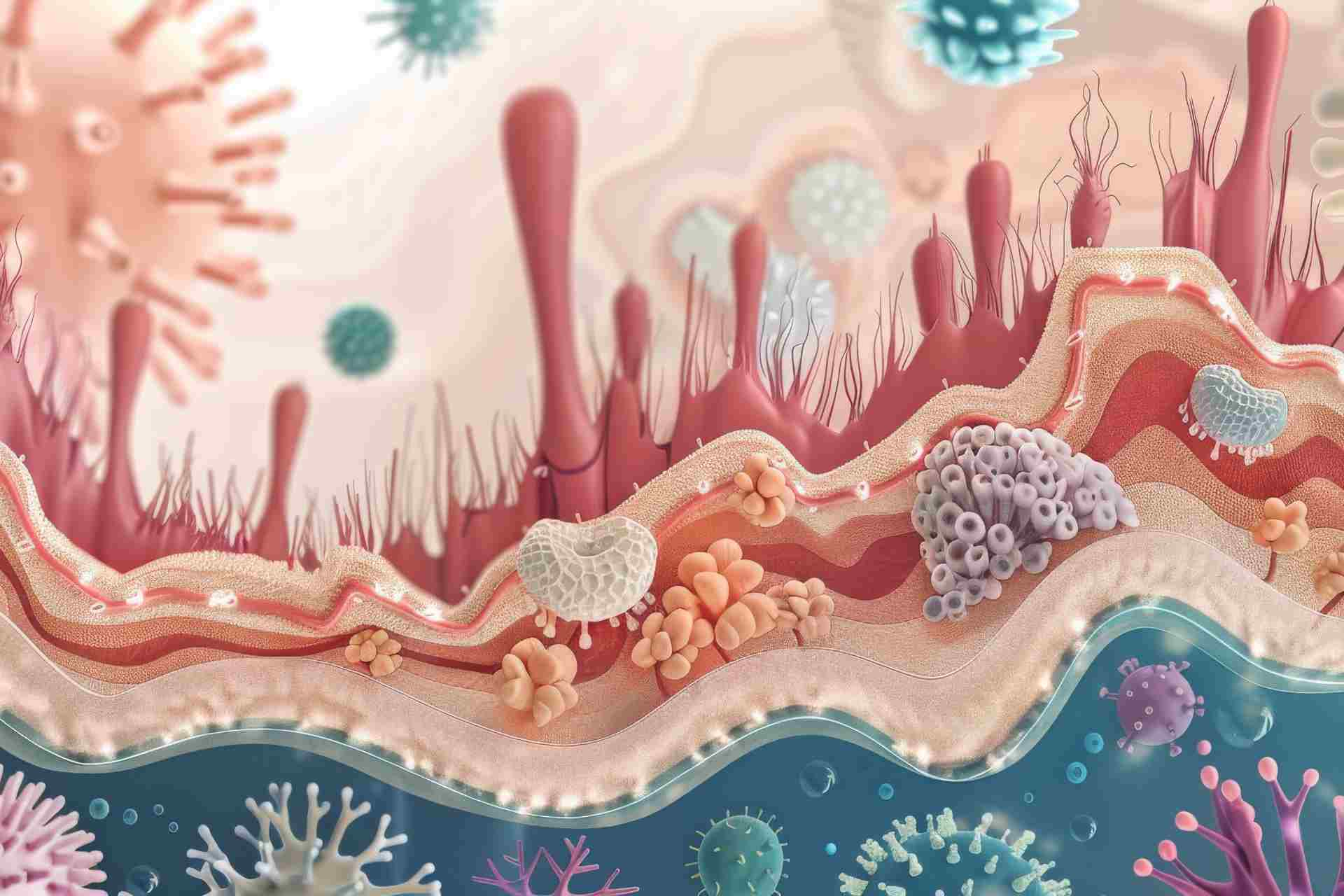
Despite improved hygiene measures, infections that occur in the wound following an invasive surgical procedure remain a leading cause of post-surgery complications. New research shows that most of these infections are caused by harmless bacteria that inhabit the patients’ skin.
The findings, published in Science Translational Medicine, may help clinicians to select more targeted antimicrobials based on where on the body the surgery is taking place or which type of bacteria inhabit that body site.
Surgical site infections occur following about 1 in 30 procedures, typically with no explanation. But where these infections come from and why they’re so resistant to antibiotics is unclear.
To better understand how and why surgical site infections happen, researchers led by Dustin Long at the University of Washington School of Medicine in Seattle analyzed samples of bacteria from the noses, skin, and stool of more than 200 patients before they underwent spine surgery — an umbrella term for surgical procedures performed on the spine to address various spinal conditions. On the day of surgery, the team also collected skin swabs from the site of the incision.
Post-surgery infection
After collecting microbial samples from the patients, the researchers followed them for 90 days to compare the initial samples with any infections that occurred following surgery.
Although the types of bacteria inhabiting the skin on the patients’ backs varied from person to person, microbes residing around the neck and shoulders were similar to those found in the nose, while microbes typically found on the lower back resembled those in the gastrointestinal tract and stool.
The way these bacteria spread on the skin matched up with how often infections happen after surgery on the same parts of the spine, the researchers found.
Skin bacteria
About 86% of post-surgery infections originated from bacteria that were already present on the patients’ skin before surgery. Nearly 60% of these infections were also resistant to the antibiotics used during the surgical procedure, the antiseptic used to clean the skin before incision, or both.
The findings suggest that most surgical site infections originate from the patient’s skin microbes, prompting a need for personalized prevention strategies. While current protocols focus on maintaining sterility in hospitals, individualized approaches could benefit patients more, the authors say.
“If these findings are replicated in other procedural cohorts, this model of [surgical site infection] pathogenesis could drive important shifts in infection prevention strategy and enable more individualized and patient-centered approaches.”