• Obesity-related changes
• Environmental effects
What is already known on this topic
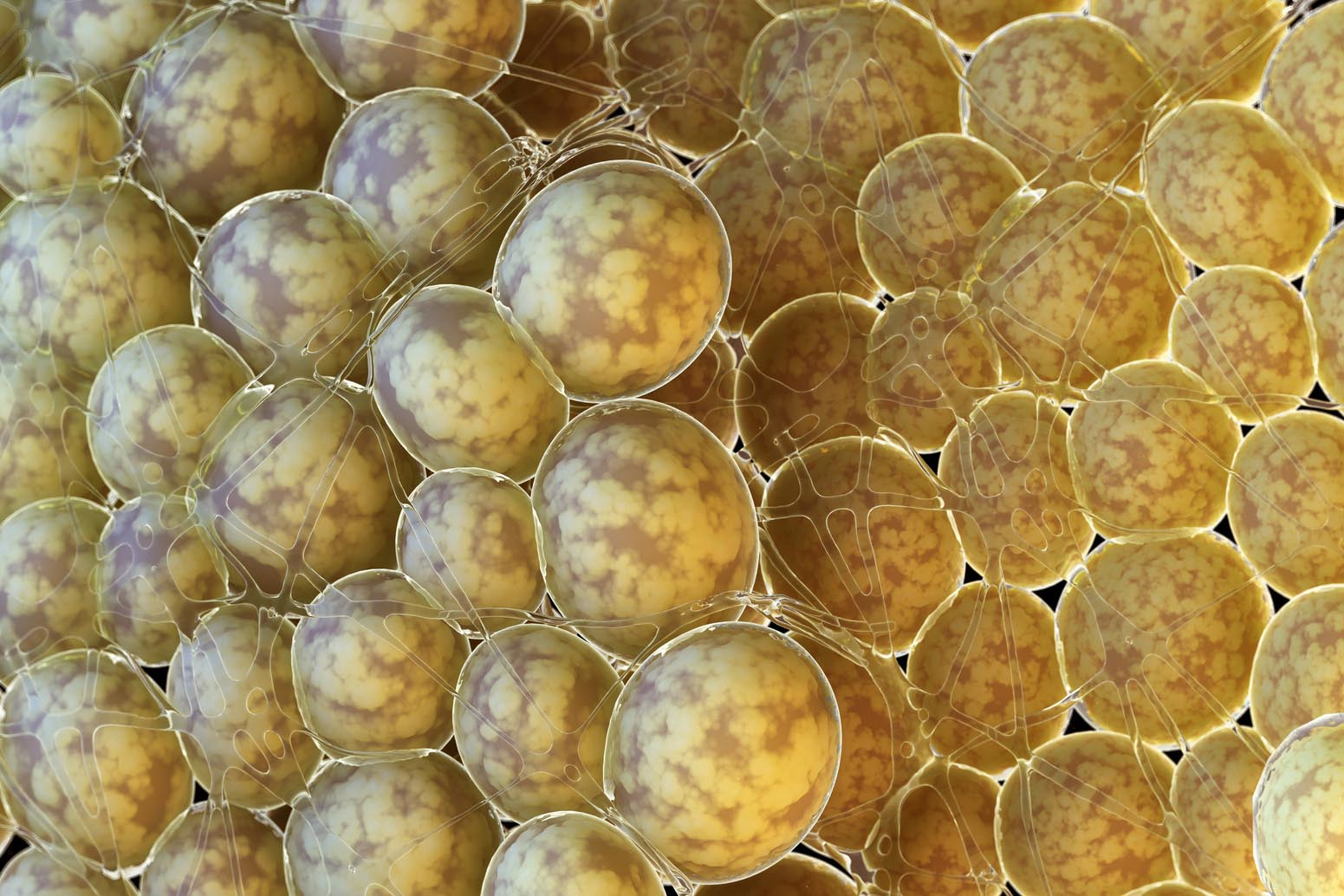
Obesity and type 2 diabetes are metabolic disorders linked to changes in the gut microbiota. But their co-occurrence poses challenges in identifying microbial signature unique to each condition.What this research adds
By analyzing the gut microbiota of lean non-diabetic, obese non-diabetic, and obese individuals with type 2 diabetes, researchers found that obesity was associated with changes in microbiota composition, including decreased Akkermansia, Faecalibacterium, Oscillibacter, and Alistipes species. But these alterations were modest for people with type 2 diabetes. Dietary supplements and drugs, including antidiabetics, were also associated with changes in microbiota composition.Conclusions
The findings differentiate microbial features of obesity and type 2 diabetes, and identify dietary
and medication exposures that should be considered in future studies.
Obesity, unlike type 2 diabetes, is associated with changes in gut microbiota composition, and dietary supplements and key medications such as antidiabetics are also linked to microbiota alterations. That’s the conclusion of a study that looked at the gut microbes of more than one thousand people, including lean and obese individuals with and without type 2 diabetes.
Obesity and type 2 diabetes are metabolic disorders linked to changes in the gut microbiota. But their co-occurrence poses challenges in identifying microbial signature unique to each condition.
The new study, led by Louise Thingholm at Christian-Albrechts-University of Kiel and published in Cell Host & Microbe, is one of the first to disentangle the microbial features of these co-occurring conditions.
Obesity-related changes
The researchers analyzed the gut microbiota of 1,280 people, including lean non-diabetic, obese non-diabetic, and obese individuals with type 2 diabetes. All the individuals studied were part of the Northern German cohorts PopGen and Focus, which have recorded information on the use of drugs and dietary supplements, as well as data on age, gender, body mass index, and fasting glucose levels.
In obese people, the team observed changes in the gut microbiota composition, including decreased levels of Akkermansia, Faecalibacterium, Oscillibacter, and Alistipes bacteria. The anti-inflammatory species Faecalibacterium prausnitzii and Bacteroides thetaiotaomicron were decreased in obese individuals but not in people with type 2 diabetes.
These associations with the microbiota were modest for people with type 2 diabetes, and included increases in Escherichia/Shigella bacteria.
Environmental effects
The researchers also found that five main medication classes, including analgesics, antihypertensives, and antidiabetics, were associated with changes in the gut microbiota structure and function.
What’s more, the use of dietary supplements including vitamins and minerals such as iron and calcium was linked to microbiota alterations.
While single medications and dietary supplements appear to be weakly associated with these microbial changes, the total effect of several drugs and supplements can be substantial. These effects should be considered in future studies, the researchers say.