What is already known
Several studies have suggested that oxidative stress and gut microbial disturbances can trigger inflammatory bowel disease (IBD), a term for two conditions that are characterized by chronic inflammation of the gastrointestinal tract. One treatment approach involves delivering small snippets of RNA called small interfering RNA, or siRNA, which inhibit the expression of certain genes that code for inflammatory proteins such as TNF-α. However, the delivery method of siRNA doesn’t ensure that the medicine reaches the colon.
What this research adds
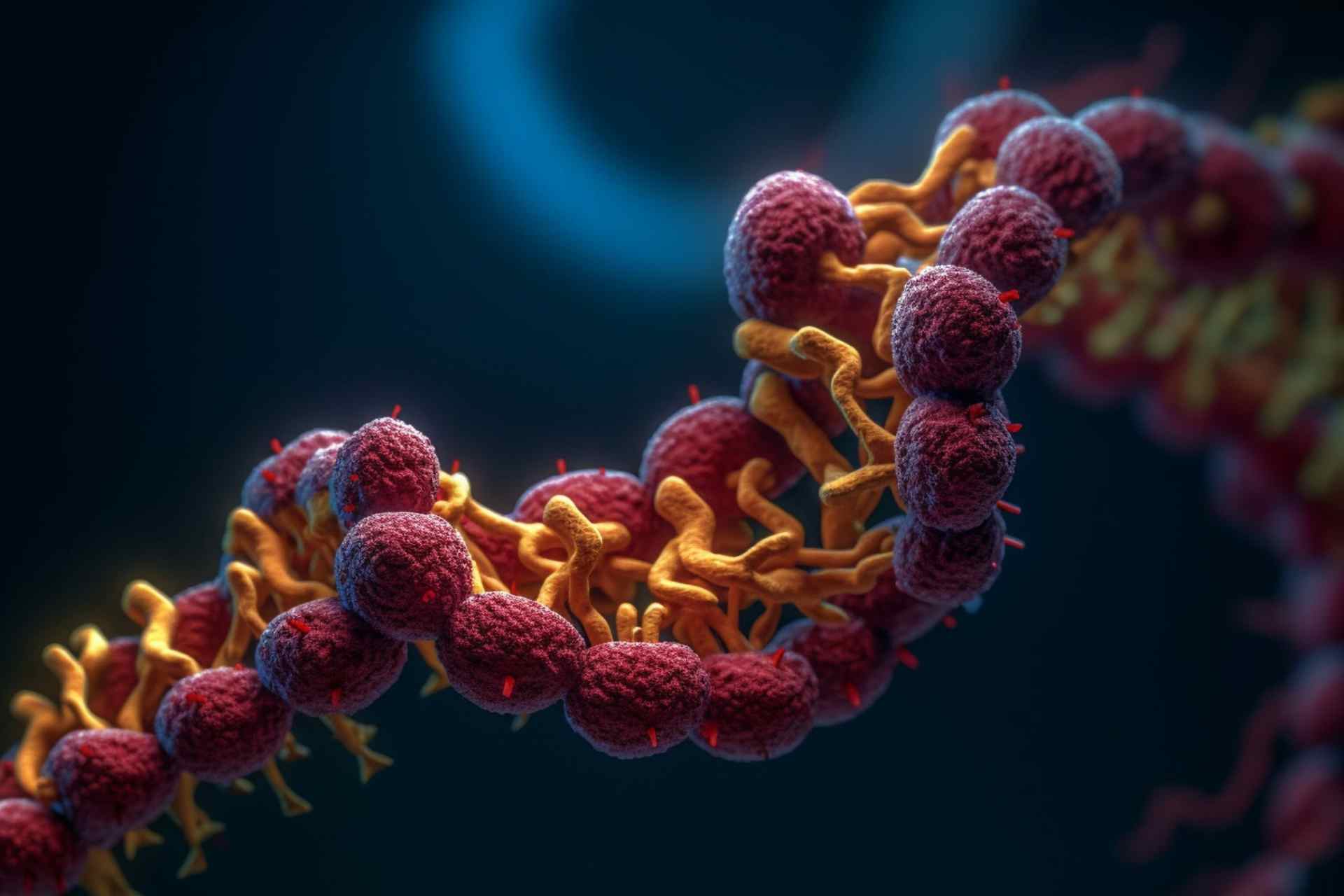
Researchers developed a nanomedicine that combines TNF-α-siRNA with polyphenol, a plant metabolite with prebiotic, antioxidant, and anti-inflammatory properties. The siRNAs are encapsulated in a multilayer shell of chitosan and tannin acid materials, which resist the harsh environment of the gastrointestinal tract and adhere to the inflamed gut. When tested in mice with IBD, the nanomedicine helped tissue repair and reduced inflammation. It also promoted the growth of beneficial gut bacteria and decreased the expression of the neurotransmitter GABA.
Conclusions
The findings suggest that the new nanomedicine approach can improve the delivery of TNF-α-siRNA in people with IBD.
Inflammatory bowel disease, or IBD, is a term for two conditions that are characterized by chronic inflammation of the gastrointestinal tract. Now, researchers have developed a new approach that may improve the delivery of treatments for IBD.
The approach, detailed in Science Advances, provides “a universal, powerful platform for the design of oral nanomedicines for inflammatory diseases,” the researchers say.
Several studies have suggested that oxidative stress and gut microbial disturbances can trigger IBD. One treatment approach involves delivering small snippets of RNA called small interfering RNA, or siRNA, which inhibit the expression of certain genes that code for inflammatory proteins such as TNF-α. But the delivery method of siRNA doesn’t ensure that the medicine reaches the colon.
“Oral administration is a convenient, safe, and desirable route for treating IBD,” the researchers say. “However, IBD-induced diarrhea can lead to rapid drug clearance.”
To overcome this challenge, Huan He at Southwest Jiaotong University in Chengdu, China, and his colleagues set out to develop an approach that makes oral delivery of TNF-α-siRNA a more viable option for people with IBD.
New design
First, the researchers combined TNF-α-siRNA with polyphenol, a plant metabolite with prebiotic, antioxidant, and anti-inflammatory properties. Then, they encapsulated the siRNAs in a multilayer shell of chitosan and tannin acid materials, which can resist the harsh environment of the gastrointestinal tract.
Cells grown in a dish were able to take up the nanomedicine, which reduced inflammation by suppressing inflammatory immune cells and activating anti-inflammatory ones.
In environments that simulate the colon, the thick ‘armor’ of chitosan and tannin acid materials prevented the degradation of the nanomedicine and prolonged its retention time, the researchers found.
Treating colitis
When tested in mice with IBD, the nanomedicine helped tissue repair and reduced inflammation. It also promoted the growth of beneficial gut bacteria and decreased the expression of the neurotransmitter GABA. This finding suggests that the nanomedicine could affect the gut-brain axis.
Indeed, mice treated with the nanomedicine also showed less anxiety- and depression-like symptoms as well as improved learning and memory in behavioral tests, the researchers found.
“In short, [the nanomedicine] alleviated colitis and ameliorated IBD-induced mood disorders and cognitive impairments,” the authors say.