What is already known
Immunotherapy has proved effective in many cancer types, and several studies have suggested that gut microbes can sway a person’s response to this type of therapy. However, immunotherapy is not a successful approach to treat pancreatic cancer, and how the microbiota may contribute to this failure is unclear.
What this research adds
Researchers screened bacterial metabolites in mice with pancreatic tumors and assessed how they affected the success of immunotherapy. They found that a molecule called trimethylamine N-oxide (TMAO) and its precursor trimethylamine (TMA) boosted anti-tumor effects. Giving TMAO or TMA to mice with pancreatic cancer delayed tumor growth by activating specific immune responses. TMAO also improved immunotherapy’s efficacy in those mice. Bacteria that produce an enzyme that generates TMA were present at higher levels in people who survived for a long period of time after pancreatic cancer compared to those who survived for only a short period of time.
Conclusions
The findings suggest that TMAO is a driver of anti-tumor immunity. Targeting TMAO may help improve the efficacy of immunotherapy in people with pancreatic cancer.
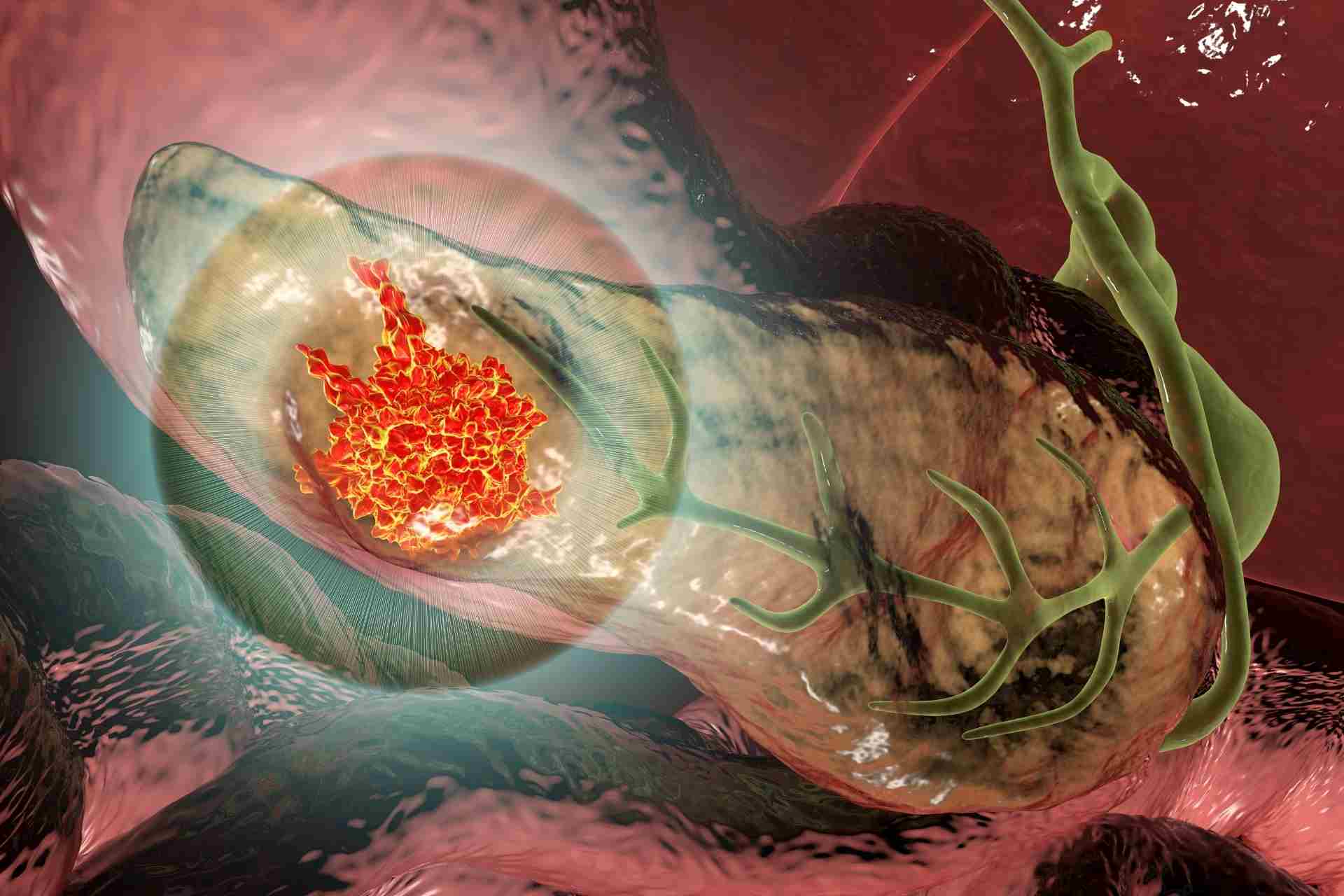
Immunotherapy has proved effective in many cancer types, but it’s not yet successful in treating other types of cancer, such as pancreatic tumors. Now, researchers have found that a gut microbial metabolite called trimethylamine N-oxide, or TMAO, could improve immunotherapy success in pancreatic cancer.
The findings, published in Science Immunology, suggest that TMAO is a driver of anti-tumor immunity. Targeting TMAO may help improve the efficacy of immunotherapy in people with pancreatic cancer.
Several studies have suggested that gut microbes can sway a person’s response to immunotherapy. However, how the microbiota may contribute to the failure of immunotherapy to treat pancreatic tumors is unclear.
Since the pancreas facilitates digestion in the gut, which hosts gut bacteria, Rahul Shinde at the Wistar Institute and his colleagues set out to explore new ways to harness gut microbes to improve immunotherapy’s efficacy in pancreatic cancer.
Anti-cancer effect
The researchers screened gut bacteria’s metabolites in mice with pancreatic tumors. Then, they investigated how these metabolites affected the success of immunotherapy.
They found that TMAO and its precursor trimethylamine (TMA) boosted anti-tumor effects. Scientists have known that dietary choline or L-carnitine, which are found in foods such as meat and eggs, are metabolized by the gut microbiota into TMA in the intestine. Then, TMA enters the blood circulation and is transformed into TMAO in the liver.
Giving TMAO or TMA to mice with pancreatic tumors delayed tumor growth, the researchers found. This is likely because TMAO and TMA activate specific immune cells such as macrophages and CD8 T cells, which can kill cancer cells. TMAO and TMA also appeared to decrease the levels of immunosuppressive markers in the tumor environment.
Improving immunotherapy
Next, the team combined TMAO administration with immunotherapy in mice with pancreatic cancer. TMAO boosted the efficacy of immunotherapy in the animals, improving their survival.
To validate the findings in humans, the researchers examined whether the presence of bacteria producing an enzyme that generates TMA was associated with positive immunotherapy outcomes in people with pancreatic cancer. These bacteria, which include Bacillus and Paenibacillus species, were present at higher levels in people who survived for a long period of time after pancreatic cancer compared to those who survived for only a short period of time, the researchers found. Bacillus bacteria are also abundant in melanoma patients who respond to immunotherapy, the authors say.
“Together, our study identifies the gut microbial metabolite TMAO as a driver of anti-tumor immunity and lays the groundwork for potential therapeutic strategies targeting TMAO,” they say.