• Diarrheal trigger
• Dangerous association
What is already known on this topic
Infections by Clostridioides difficile (C. difficile), which can cause life-threatening inflammation of the gut, have been traditionally associated with hospitalization and antibiotic use. But recent studies show increasing rates of C. difficile infection among people not considered to be at high risk.What this research adds
Researchers analyzed surveys of the gut microbiota of individuals who had diarrhea and were not treated with antibiotics, and then the team tested the association between diarrhea and C. difficile infection in mice. The results show that diarrheal events, such as those triggered by food poisoning and laxative abuse, can increase susceptibility to C. difficile infection.Conclusion
The study suggests that diarrheal events create a window of susceptibility to C. difficile infection, and the development of new therapies that aim to increase colonization resistance during this window could help to reduce the prevalence of C. difficile.
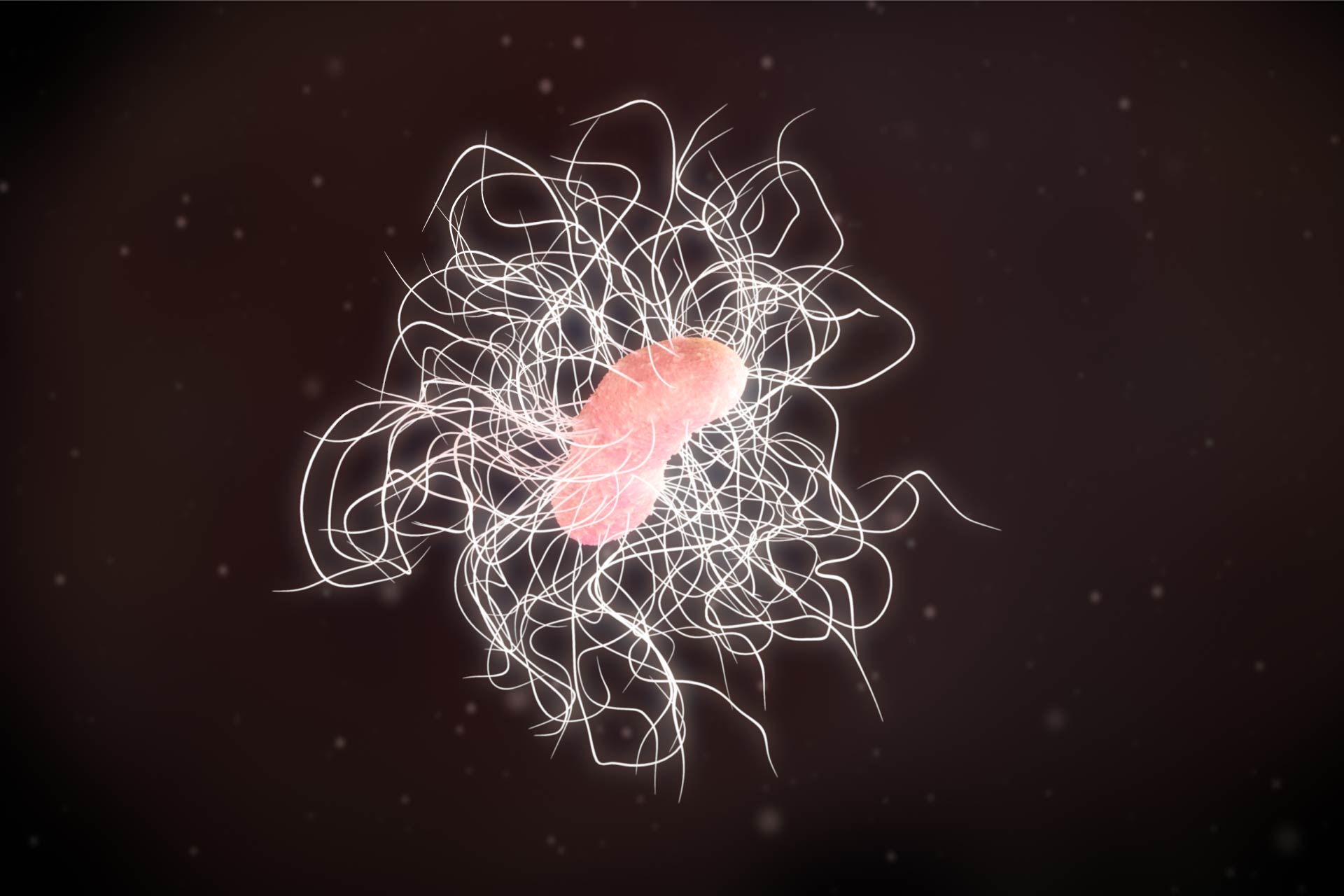
Infections by Clostridioides difficile (C. difficile), which can cause life-threatening inflammation of the gut, have been traditionally associated with hospitalization and antibiotic use. But recent studies show increasing rates of C. difficile infection among people not considered to be at high risk. Now, a study in mice has shown that events that trigger diarrhea, such as food poisoning and laxative abuse, can increase susceptibility to C. difficile infection.
The findings, published in Nature Microbiology, show that the risk of colonization with C. difficile is highest during recovery from acute diarrhea. “Roughly 48 million people contract a foodborne illness every year in the United States, highlighting the days immediately following illnesses like these as a substantial target for reducing the prevalence of C. difficile,” the researchers say.
To determine whether diarrhea triggers colonization by C. difficile, David VanInsberghe at the Massachusetts Institute of Technology in Cambridge and his colleagues analyzed previous studies that surveyed the gut microbiota of people who had diarrhea, caused by either food poisoning or Vibrio cholerae infection. None of the individuals was treated with antibiotics.
Diarrheal trigger
The researchers observed that C. difficile infection occurred as people recovered from diarrheal illnesses, and individuals remained colonized with C. difficile for up to a year. The number of C. difficile bacteria shed in a carrier’s stool was variable and could increase by more than 1,000 times in one day, likely influencing the transmissibility of C. difficile outside of hospitals.
These results underscore that C. difficile infection is not a common hospital transmission, VanInsberghe says. “In our study, two of the people we followed with high temporal resolution became carriers outside of the hospital.”
Next, the team set out to study surveys of the microbiota of people who did not have recent diarrhea. The researchers found that C. difficile was rare in these individuals, further suggesting that diarrhea facilitates C. difficile colonization.
Dangerous association
To test the association between diarrhea and C. difficile infection, the team fed mice increasing quantities of laxatives while exposing them to C. difficile spores, and then monitored the animals’ feces for C. difficile blooms.
Mice treated with high quantities of laxatives had more C. difficile blooms in their feces than those treated with lower quantities of laxatives. Mice that weren’t given laxatives had no detectable C. difficile in their stool.
The findings suggest that diarrheal events create a window of susceptibility to C. difficile infection, and the development of new therapies that aim to increase colonization resistance during this window could help to reduce the prevalence of C. difficile, the researchers say.
“I believe that there is a lot of rethinking of C. diff infections at the moment and I hope our study will help contribute to ultimately better manage the risks associated with it,” says study senior author Martin Polz.