• Relieving symptoms
• Treating celiac disease
What is already known on this topic
Celiac disease is an immune reaction to eating gluten, a protein found in some cereals including wheat and barley. Although 40% of the global population expresses celiac disease susceptibility genes, only 1% develops the disorder. This suggests a role for environmental factors, including the gut microbiota. But the relationship between celiac disease and gut microbes remains unclear.What this research adds
Working in mice, researchers have found that a microbial-derived metabolite of the dietary amino acid tryptophan binds to receptor proteins that can trigger immune responses in the gut. In mice that express a celiac disease susceptibility gene, the suboptimal activation of this receptor promoted celiac disease inflammation. However, a diet rich in tryptophan as well as treatment with bacteria such as Lactobacillus reuteri helped to reduce gluten-related inflammation.Conclusion
The findings could point to new molecular targets or potential dietary strategies to treat celiac disease.
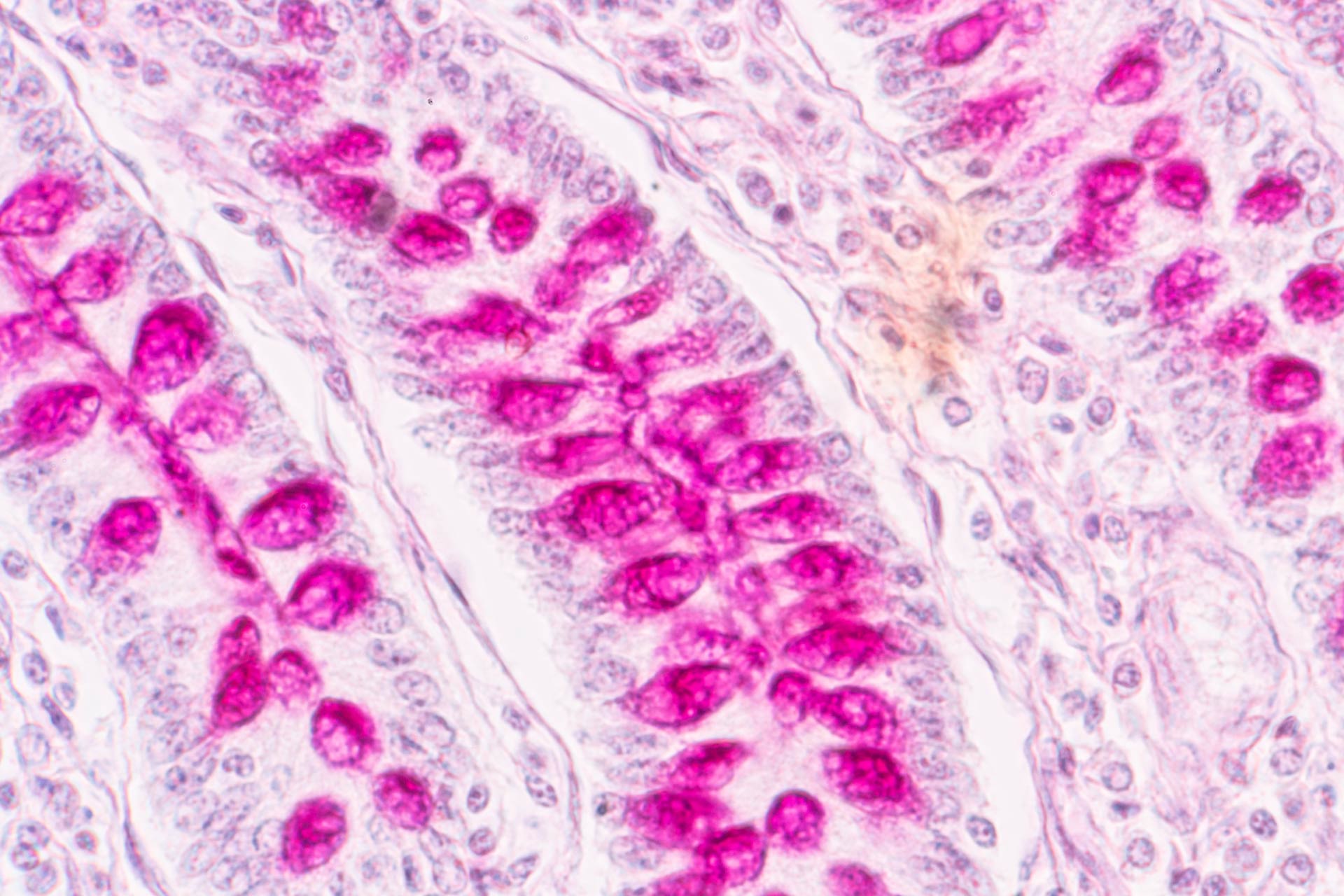
Celiac disease, an immune reaction to a protein found in some cereals, is caused by a combination of genetic and environmental factors. Now researchers discovered that the breakdown of dietary tryptophan by gut bacteria is altered in mice with the disease.
The findings, published in Science Translational Medicine, could help to explain why 40% of the global population expresses celiac disease susceptibility genes, but only 1% develops the disorder. They also highlight a potential strategy for treating the condition.
“The only treatment for celiac disease is a strict adherence to a gluten-free diet, which is difficult to follow, and doesn’t always lead to complete recovery of the gut or symptom resolution,” says study co-senior author Elena Verdu at McMaster University in Hamilton, Canada.
Scientists have known that some gut bacteria are able to metabolize tryptophan, an essential amino acid that is found in foods including poultry, bananas and vegetables such as broccoli and cabbage. By breaking down dietary tryptophan, intestinal microbes produce metabolites that bind to receptor proteins in the gut. One of these receptors is called aryl hydrocarbon receptor (AhR) and its suboptimal activation has been linked to inflammatory bowel diseases.
So Verdu and her colleagues set out to investigate whether tryptophan metabolism was altered in the gut of mice that express a celiac disease susceptibility gene.
Relieving symptoms
Celiac disease-prone mice were exposed to gluten and then subjected to three interventions aimed at enhancing the activation of AhR.
The researchers found that a diet rich in tryptophan shifted the microbiota composition in the rodents to produce more molecules that are able to bind to AhR, in turn reducing gluten-related inflammation.
Treatment with bacteria, including Lactobacillus reuteri, that produce AhR ligand molecules also relieved celiac inflammation in the rodents’ gut. Similar results were observed after treating mice with a drug called Ficz, which boosts AhR activity.
Treating celiac disease
Next, the team analyzed stool samples from people with celiac disease. Compared to healthy people and those with the disease in remission from a gluten-free diet, individuals with active celiac disease produced fewer AhR ligand molecules and showed impaired intestinal AhR pathway activation.
The findings suggest that celiac disease is associated with a reduced capacity of the gut microbiota to metabolize tryptophan. They also point to the potential therapeutic value of targeting tryptophan metabolism in the gut to better control symptoms of celiac disease.
“Our results should prompt interventional studies in this patient group to evaluate tryptophan supplementation in combination with probiotic organisms, such as L. reuteri strains, that produce AhR ligands from the dietary substrate,” the researchers say. “This therapeutic approach could also be useful as a preventative strategy in at-risk populations.”