What is already known
Scientists have been trying to ease or treat conditions such as obesity and inflammatory bowel disease using live bacterial therapeutics. The idea behind this approach is to engineer bacteria to produce compounds able to restore a healthy microbiota or address genetic errors of metabolism. However, bacterial strains grown in the lab cannot compete with the native gut bacteria that are well adapted to their host.
What this research adds
Researchers collected Escherichia coli from the gut microbiota of mice and engineered them to express a gene of interest. Then, they reintroduced the engineered bacteria into a mouse host. For example, the team engineered E. coli to produce a protein called bile salt hydrolase (BSH), which is thought to affect host metabolism. After a single treatment, E. coli producing BSH were present throughout the gut of mice and reduced diabetes progression.
Conclusions
The findings suggest that engineered native gut bacteria could be employed to help treat certain diseases such as diabetes.
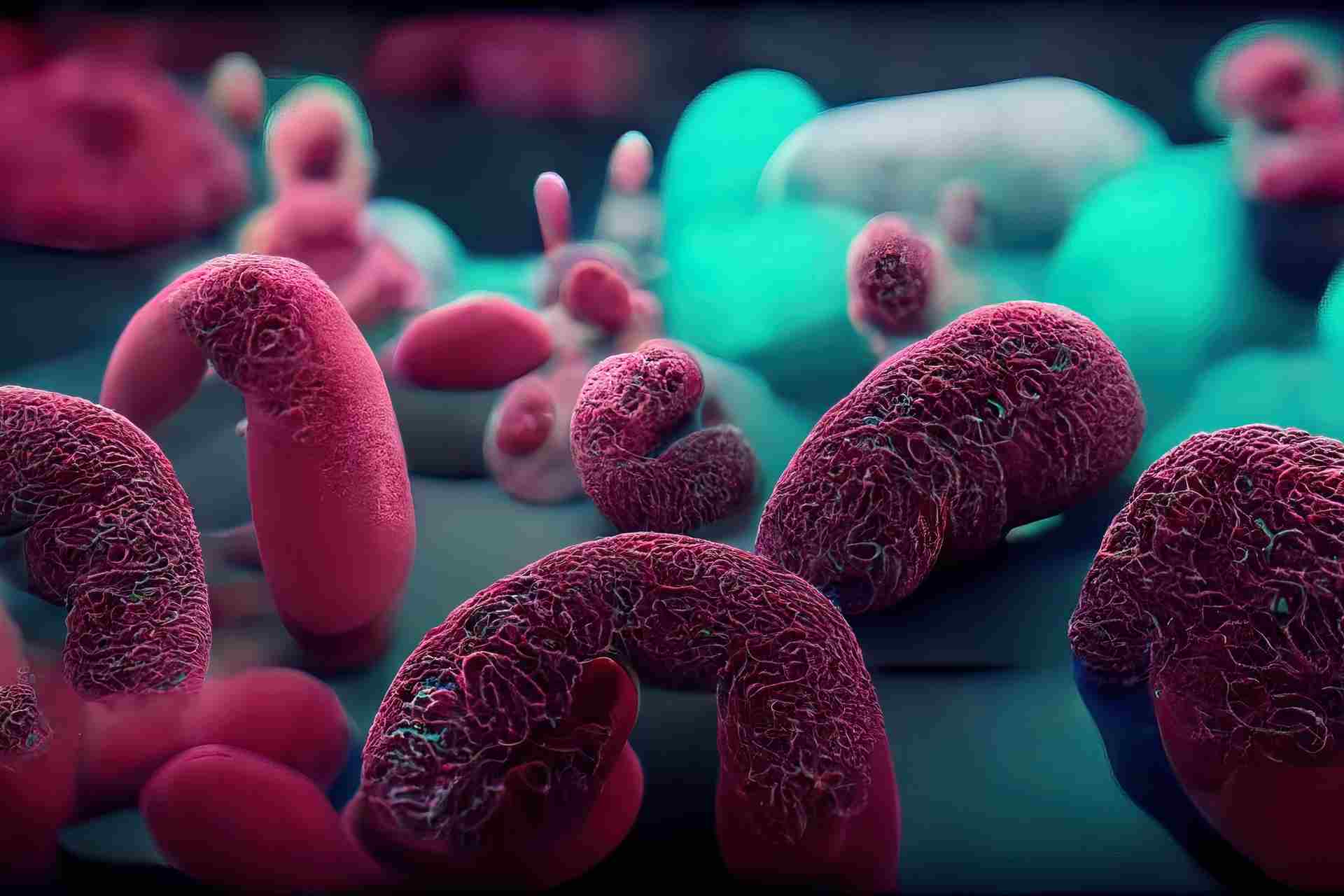
Conditions such as obesity and inflammatory bowel disease are associated with alterations of the gut microbiota. New research done in mice suggests that engineered native gut bacteria could be employed to help treat some of these diseases.
The findings, published in Cell, may inform the development of microbiota therapy for several chronic and genetic diseases, the researchers say.
Scientists have been trying to ease or treat microbiota-associated conditions using live bacterial therapeutics. The idea behind this approach is to engineer bacteria to produce compounds able to restore a healthy microbiota. Bacteria can also be engineered to express functions that address genetic errors of metabolism, for example the metabolism of an amino acid called phenylalanine in people with phenylketonuria — a rare genetic disorder that causes phenylalanine to build up in the body, leading to intellectual disability, seizures and other symptoms.
Efforts to develop live bacterial therapeutics have focused on using bacterial strains from the Bacteroides and Lactobacillus families, or Escherichia coli bacteria grown in the lab. However, lab-grown microbes cannot compete with the native gut bacteria that are well adapted to their host.
To overcome this challenge, a team of researchers led by Amir Zarrinpar at the University of California, San Diego, engineered members of the gut microbiota to express genes that could help ease symptoms of specific conditions.
Slowing down diabetes
The researchers collected stool samples from healthy mice and isolated strains of Escherichia coli from the animals’ gut microbiota. The team then engineered the bacteria to express specific genes of interest. Next, they reintroduced the engineered bacteria into a mouse host.
Engineered E. coli could colonize the whole gut of mice and survive there for the entire lifetime of the host. To assess whether the bacteria could also help to ease symptoms of disease, the researchers engineered them to produce a protein called bile salt hydrolase (BSH), which is thought to affect host metabolism.
After a single treatment, E. coli producing BSH colonized the gut of mice and changed the animals’ gut metabolites without altering their microbiotas. The engineered bacteria also improved the mice’s insulin sensitivity and glucose tolerance, reducing diabetes progression.
Engineering human microbes
Finally, the researchers set out to assess whether their approach could be used in humans. To do so, they isolated E. coli strains from gut biopsies of people undergoing routine endoscopy.
Human gut bacteria could be modified to express a gene of interest, the researchers found. However, they say, “further studies are necessary to determine whether the autologous transfer of engineered native bacteria can lead to long-lasting colonization of a human host and treatment of long-standing chronic conditions and genetic diseases.”
The findings suggest that inserting a gene into native gut microbes is much more difficult than doing so with lab-grown bacteria, but Zarrinpar’s team is working towards optimizing this process. “There are many new genetic engineering tools available now that will allow us to engineer these bacteria more effectively,” he says.